Ann Thorac Surg:胸导管旁淋巴结--新概念?
2018-04-06 Rock CardiothoracicSurger
胸导管切除是常规en bloc纵隔食管癌切除的一部分。随着微创技术的适应,很多中心开始原位保留胸导管。然而,前期的研究表明该区域存在胸导管淋巴结,并可出现转移。
胸导管切除是常规en bloc纵隔食管癌切除的一部分。随着微创技术的适应,很多中心开始原位保留胸导管。然而,前期的研究表明该区域存在胸导管淋巴结,并可出现转移。
但是,由于不同研究的手术和解剖方式不同,所报道纵隔淋巴结部位、数量等并不明确,鉴于此,来自瑞士的Bernadette Schurink教授等开展了一项研究,该研究旨在评估胸导管周围脂肪组织中的淋巴结数量、位置等信息。
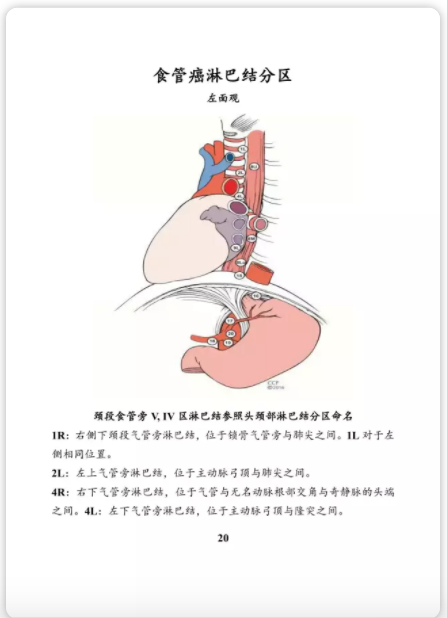
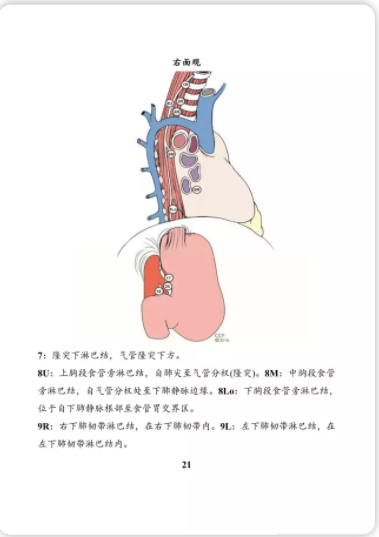
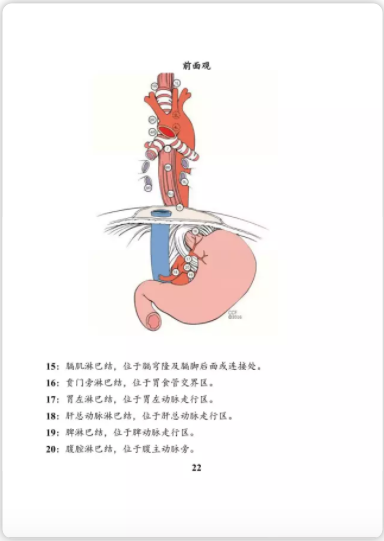
第八版食管癌淋巴结,然而并无胸导管旁淋巴结的定义
研究者在7例新鲜冷冻尸体上进行经右胸腔镜食管切除术(男性3例;女性4例)。手术中将食管和7,8和9组淋巴结整块切除,然后切除覆盖主动脉的剩余脂肪组织,将胸导管和胸导管淋巴结一并切除。淋巴结通过苏木素-伊红染色观察,并从宏观和微观上进行计数。
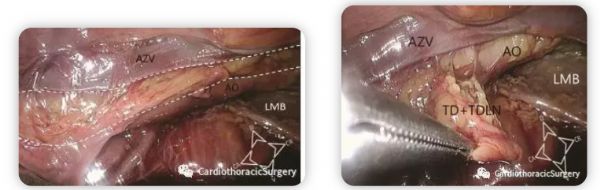
胸导管旁淋巴结解剖示意图
研究者发现,6/7(86%)例尸体上发现胸导管淋巴结,中位数为1(范围0-6)。淋巴结主要位于奇静脉区域。中位隆突下淋巴结为4个(1-8),食管旁淋巴结为2个(1-4)。
术中图片
所以研究者认为,胸导管淋巴结主要位于胸导管周围的脂肪组织内。所以在食管切癌切除术中应重视增加该区域淋巴结的切除。

术后病理
原始出处:
Schurink B, Defize IL, Mazza E, et al. Two-Field Lymphadenectomy During Esophagectomy: The Presence of Thoracic Duct Lymph Nodes. Ann Thorac Surg. 2018 Mar 23.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胸导管#
44
#THORAC#
42
#淋巴结#
38
不错的文章值得拥有
70
学习
63
了解一下.谢谢分享!
66