多普勒经胸超声心动图检测成人肺动脉高压
2022-05-13 刘少飞 MedSci原创
一些研究质疑无创测量肺动脉压的准确性。超声心动图诊断 PH 的准确性存在很大的不确定性。本研究将确定经胸多普勒超声心动图检测 PH 的诊断准确性。
肺动脉高压是指从心脏右半部向肺部供血的血管中的高血压。这是一种严重的情况,会损害心脏的右侧。血管壁变得厚而僵硬,使血液难以流动。这可能导致心脏衰竭。症状可能包括呼吸急促、疲倦、胸痛、心跳加快或下肢和腹部肿胀。这些症状可能与其他心脏和肺部疾病相似,所以诊断可能需要时间。早期诊断是有益的,因为治疗可以早期开始。早期开始治疗更好,因为人们在疾病的早期阶段对治疗的反应更好。不及早诊断会造成严重后果,如日常生活中的残疾或死亡。诊断肺动脉高压的最准确方法是使用一种叫做右心导管的压力测量。然而,这是一种侵入性的,并可能引起并发症。另一种技术,即多普勒超声心动图是无创的,更便宜,而且在医院里更广泛地使用。因此,许多指南推荐使用超声心动图作为初始诊断方法。我们想做这个回顾,因为有几项研究对超声心动图的准确性提出了质疑。我们想了解在诊断肺动脉高压方面,超声心动图与右心导管检查相比有多大优势。
研究目的:
评价超声心动图与右心导管检查相比,确定多普勒经胸超声心动图对疑似肺动脉高压患者检测PH的诊断准确性。
研究方法:
我们纳入了评估经胸多普勒超声心动图检测PH的诊断准确性的研究,其中右心导管检查是参考标准。我们排除了诊断性的病例对照研究。我们排除了右心导管检查不是参考标准或参考标准阈值不同于25mmHg的研究。我们排除了指数检查和参考标准之间间隔超过一周的研究,因为干预措施可能在初次检查后不久就会实施,医疗条件可能因时间不同而不同(如相隔>1周)。我们排除了没有提供足够的诊断测试准确性数据(基于参考标准的真阳性[TP]、假阳性[FP]、真阴性[TN]和假阴性[FN]值)的研究,如案例系列研究。我们纳入了提供数据的研究,从这些数据中我们可以提取基于参考标准的TP、FP、TN和FN值。我们联系了研究作者,以寻找缺失的数据。我们没有根据出版类型(如全文、致编辑的信、会议摘要或未发表的数据)来排除研究。
研究结果:
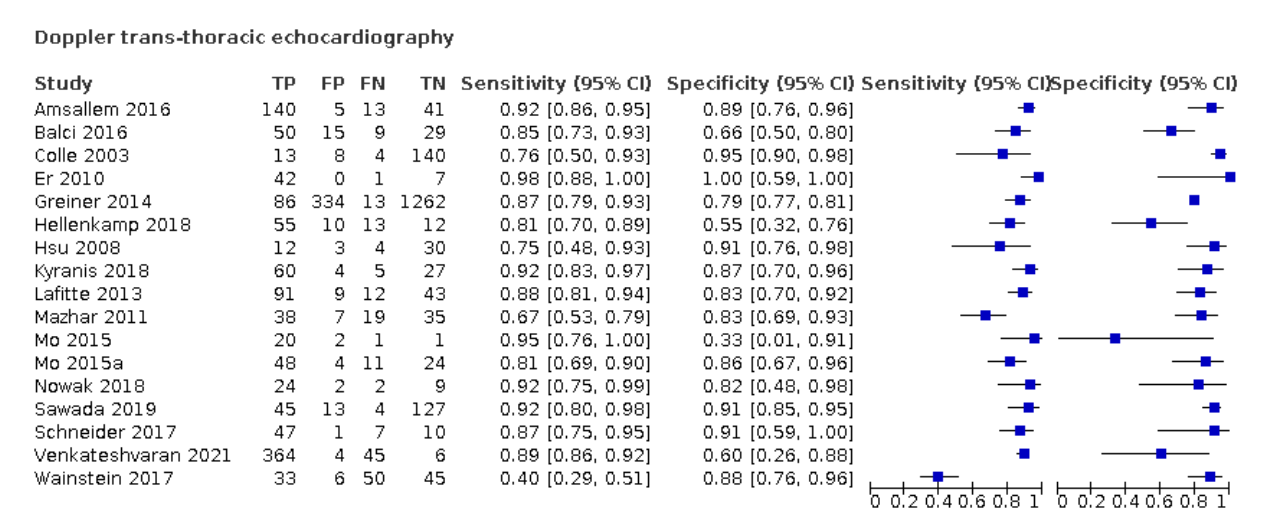
我们纳入了17项研究(包括3656名成年患者),评估多普勒经胸超声心动图诊断PH的准确性。纳入的研究在患者的年龄分布、性别、WHO分类、环境、国家、阳性阈值和发表年份等方面都是不一样的。纳入的研究报告中PH的患病率差异很大(从6%到88%)。诊断PH的指标测试阈值差异很大(从30mmHg到47mmHg),而且并不总是预先指定的。在评估的每个QUADAS-2领域中,没有研究被评为低偏倚风险或低关注度。报告不完善,特别是在指数测试和参考标准领域,阻碍了对偏倚风险的结论性判断。纳入的研究中使用的阈值几乎没有一致性;因此,常见的阈值包含非常稀少的数据,这使我们无法计算准确性估计的总结点。在固定的特异性为86%(特异性中值)的情况下,使用HSROC模型从特异性中值得出的估计灵敏度为87%(95%置信区间[CI]:78%至96%)。如果PH的发病率为68%,这是主要在三级医院进行的研究中的中位数,对怀疑有PH的1000名成年患者的队列进行诊断将导致88名患者未被诊断为PH(假阴性),275名患者将避免不必要的转诊进行右心导管检查(真阴性)。此外,1000名患者中有592名将获得适当和及时的转诊,进行右心导管检查(真阳性),而45名患者将被错误地认为患有PH(假阳性)。相反,当我们假设PH的发病率较低(10%),如肝移植的术前检查,假阴性和假阳性的数量将分别为13和126。
研究结论:
我们对成人患者超声心动图诊断PH的证据评估显示了一些局限性。我们无法确定任何特定指标测试阈值的平均敏感性和特异性,也无法解释观察到的结果差异。所收集数据的高度异质性和方法学质量差,将制约这一结果在临床实践中的实施。需要进一步研究多普勒经胸超声心动图诊断成人PH的准确性,并采用严格的方法进行诊断测试准确性研究。
参考文献:
Tsujimoto Y, Kumasawa J, Shimizu S, Nakano Y, Kataoka Y, Tsujimoto H, Kono M, Okabayashi S, Imura H, Mizuta T. Doppler trans-thoracic echocardiography for detection of pulmonary hypertension in adults. Cochrane Database Syst Rev. 2022 May 9;5:CD012809. doi: 10.1002/14651858.CD012809.pub2. PMID: 35532166.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#经胸超声心动图#
39
#心动图#
47
#动脉高压#
32
精彩评论,需要您登录查看
35
#多普勒#
36