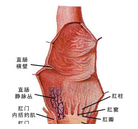
盘点:近期结直肠癌重大研究及指南共识汇总
2016-10-31 MedSci MedSci原创
我国结直肠癌的发病率和病死率均保持上升趋势。 2011年结直肠癌的发病率和病死率分别为23.03/10万和11.11/10万。其中,城市远高于农村,且结肠癌的发病率上升显著。 多数患者发现时已属于中晚期。 梅斯小编整理了近期结直肠癌重大研究及指南共识,与大家分享。【1】Ann Intern Med:粪便免疫化学测试筛查结直肠癌根据发表在Annals of Internal Medicine的一
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#重大研究#
20
哪里能下最新指南
61
满满干货!
55
结直肠癌重大研究及指南共识汇总。
67
#结直肠#
0
太有意义了
61