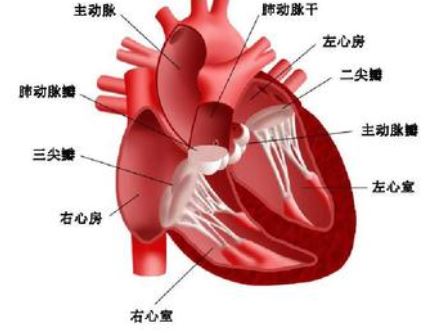
JACC:可预测主动脉瓣狭窄患者死亡率的心肌损伤标志物
2021-08-07 MedSci原创 MedSci原创
心肌纤维化和双心室重塑标志物是AS患者生存预后的主要预测指标
目前,临床上越来越多的采用心血管磁共振(CMR)进行主动脉瓣狭窄(AS)的风险分层。但是,CMR标志物及其各自阈值的相对预后作用尚不明确。
最新发表在“J Am Coll Cardiol”上的一项研究“Markers of Myocardial Damage Predict Mortality in Patients With Aortic Stenosis”,利用机器学习,以确定AS中的重要的预后CMR标志物及其死亡阈值。
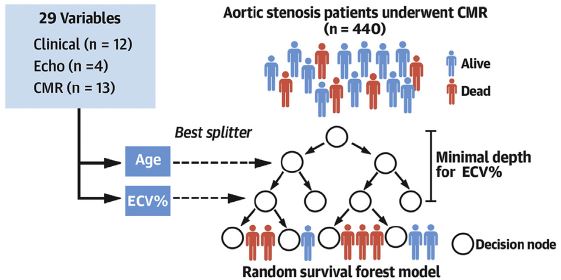
研究流程
在13个国际站点前瞻性的招募了进行AVR治疗的重度AS患者:开发队列 440位、验证队列 359位,中位随访了3.8年。在手术或经导管AVR治疗前对所有患者进行CMR。采用29个变量(13个CMR)建立以AVR后死亡为结果的随机生存森林模型。
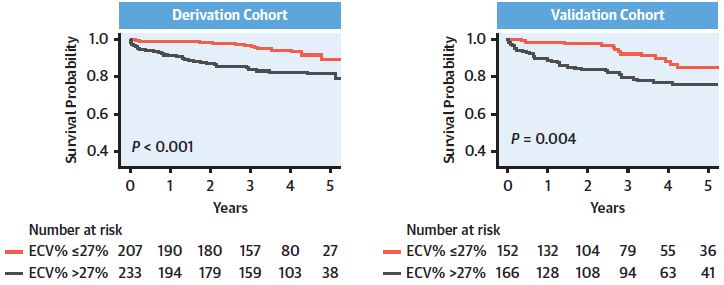
根据细胞外体积分数分层的患者存活率
开发队列和验证队列分别发生了52例和51例死亡事件。4个最具预测性的CMR指标是细胞外容积分数、晚期钆增强、左室舒张末期容积指数(LVEDVi)和右室射血分数。在整个队列和无症状患者亚组中,当细胞外体积分数超过27%时,经风险调整的预测死亡率显著增加,而晚期钆增强>2%显示持续性高死亡风险。
根据RVEF分数分层的患者存活率
大心室(LVEDVi >80 mL/m2)和小心室(LVEDVi≤55 mL/m2)以及右心室射血分数高(>80%)或低(≤50%)的患者的死亡率均有所增加。当将这4个指标加入临床因素时,模型对死亡的预测表现进一步提高(3年C指数:0.778 vs 0.739)。CMR变量的预后阈值和风险分层在验证队列中均得到了证实。
根据LVEDVi分层的患者存活率
总之,在该研究中,机器学习确定心肌纤维化和双心室重塑标志物是AS患者生存预后的主要预测指标,并强调了它们与死亡率的非线性相关性。这些标记物可能对优化AVR的判定有一定的作用。
原始出处:
Soongu Kwak, et al. Markers of Myocardial Damage Predict Mortality in Patients With Aortic Stenosis. J Am Coll Cardiol. 2021 Aug, 78 (6) 545–558
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#标志物#
38
#患者死亡#
28
#JACC#
32
点赞
46
#心肌损伤#
55
#ACC#
31
#主动脉瓣#
39
#损伤#
30
#主动脉#
35
很好,对心血管医学生有较大的指导意义
67