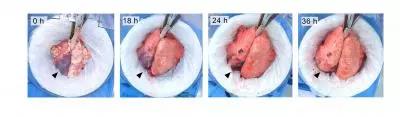
Anesthesiology:逐渐性增加潮气量可减轻大鼠实验性肺损伤
2019-06-30 佚名 罂粟花
对于轻度急性呼吸窘迫综合征,高潮气量(VT)可产生一定程度的肺损伤;本研究假设如果VT缓慢增加,可减少机械异质性并使肺泡上皮细胞和内皮细胞以及细胞外基质产生适应性,则肺损伤可以减轻。故本研究本研究旨在探讨逐渐增加潮气量的不同方式对大鼠实验性肺损伤的影响 。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#实验性#
32
#潮气量#
43
#EST#
25
#损伤#
42
#肺损伤#
34
#ESI#
30
666
87
666
74