Cell:揭示阿尔茨海默病新机制:大脑“清洁工”能量不足,无法清除蛋白斑
2017-08-16 漱石 生物探索
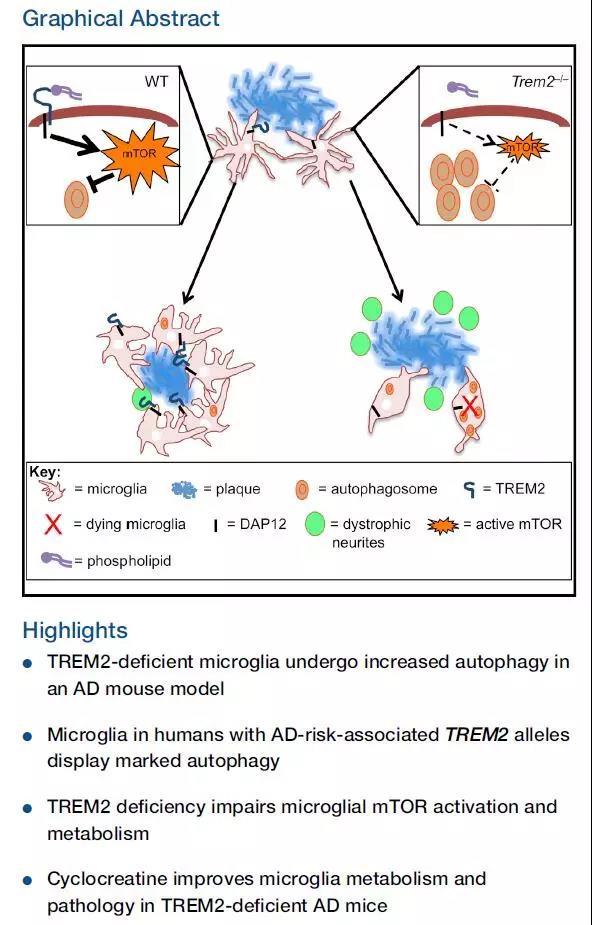
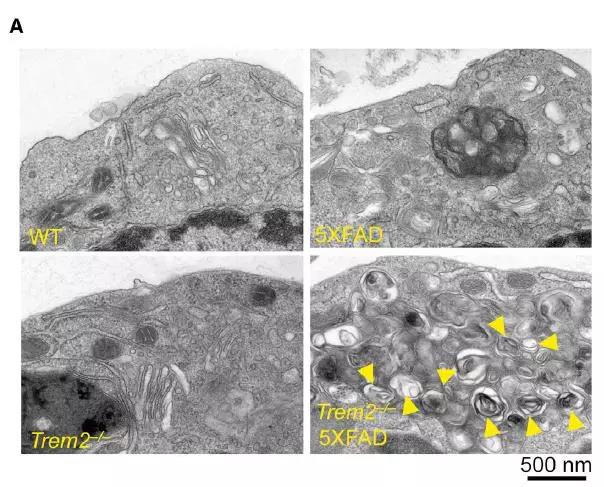
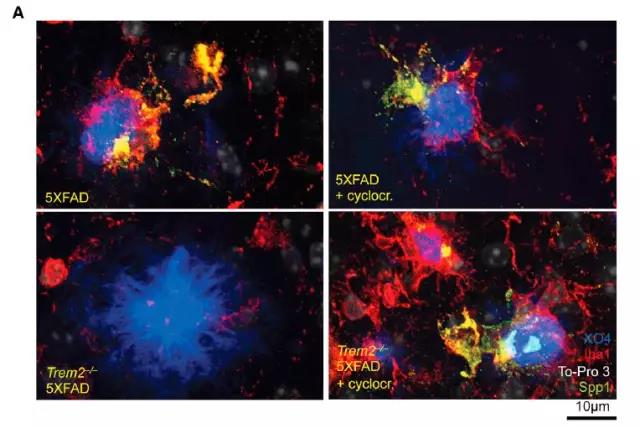
近日,华盛顿大学医学院的一项新研究表明,TREM2的高风险突变会导致大脑中的免疫细胞——小胶质细胞能量赤字。当这些细胞在能量亏空情况下工作时,它们无法有效地清除蛋白斑的积累,因而无法保护神经元免受蛋白斑的损伤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
35
#Cell#
24
#阿尔茨#
34
#阿尔茨海#
34
#阿尔茨海默#
34
学习了,谢谢。
67