p for trend内涵与SPSS实现
2019-09-24 临床流行病学和循证医学 临床流行病学和循证医学
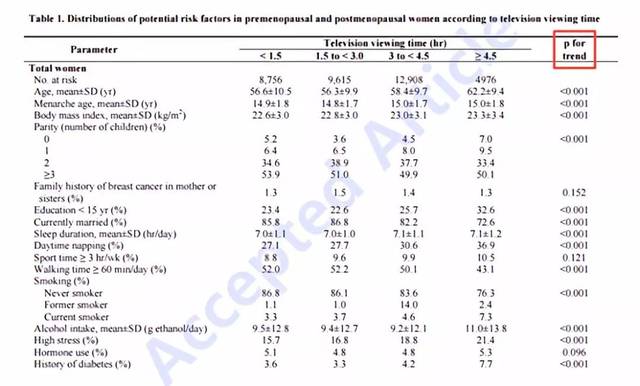
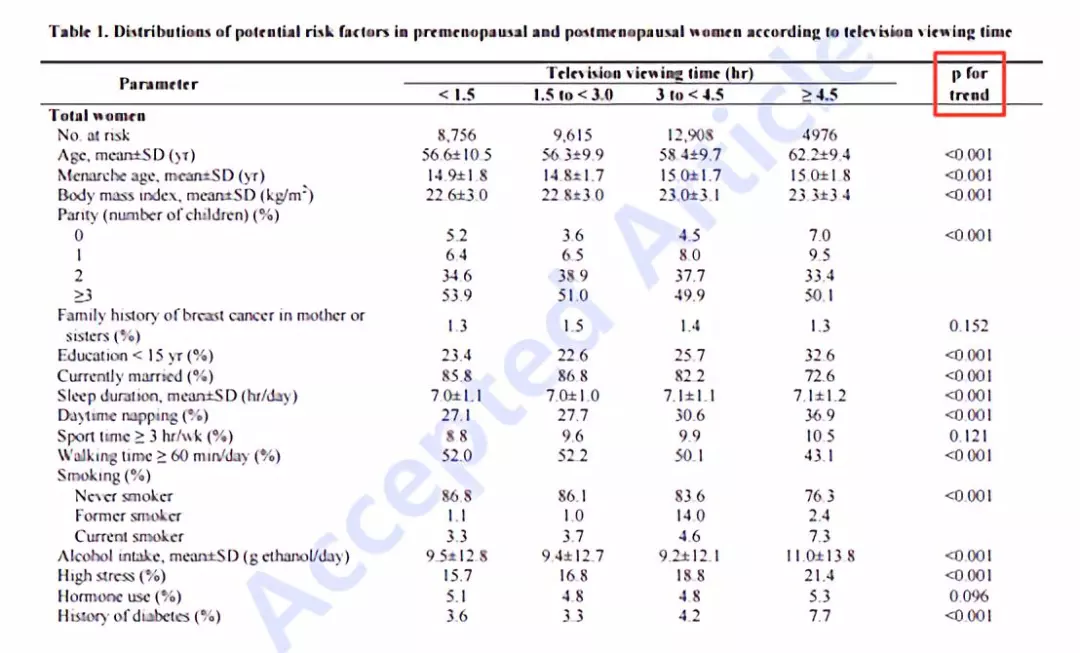
p for trend主要是指随着某分组变量的递增或递减(需要注意的是,该分组变量需是有序多分类变量),其他变量是否存在某种趋势变化。如下表中,每日观看电视时长为有序多分类变量:小于1.5h,1.5~3.0h,3.0~4.5h,大于等于4.5h。研究者探讨了随着电视观看时长的增加,其他变量的变化情况。我们知道卡方检验中的“线性关联”可以提供随着分组变量的递增,某分类变量的趋势变化。但是,随着某分组
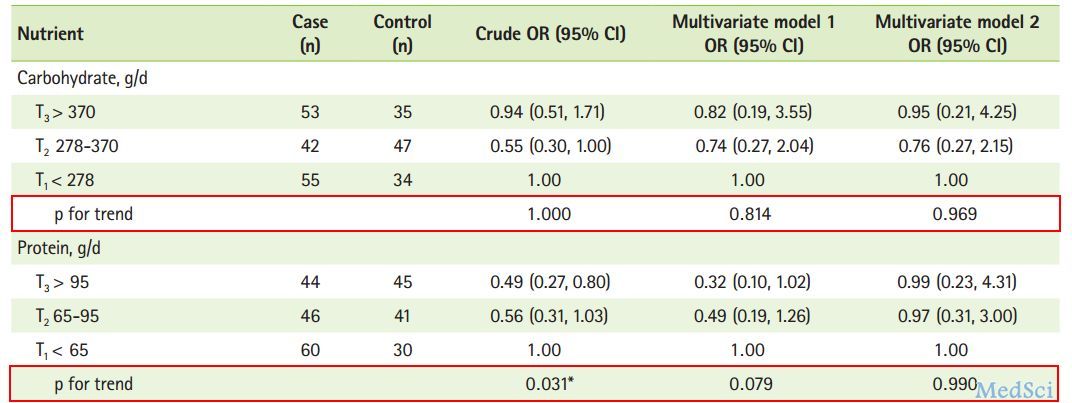
p for trend主要是指随着某分组变量的递增或递减(需要注意的是,该分组变量需是有序多分类变量),其他变量是否存在某种趋势变化。如下表中,每日观看电视时长为有序多分类变量:小于1.5h,1.5~3.0h,3.0~4.5h,大于等于4.5h。研究者探讨了随着电视观看时长的增加,其他变量的变化情况。我们知道卡方检验中的“线性关联”可以提供随着分组变量的递增,某分类变量的趋势变化。但是,随着某分组变量的递增,可以探讨某连续变量的趋势变化吗?如下表中,随着观看电视时长的递增,年龄是否存在某种趋势关系?看一个例子先,比如,我们想研究随着年龄增加,腰围和臀围的变化情况。通过描述性结果可知,随着年龄递增,腰围和臀围有增加的趋势。但是这种趋势是否有统计学意义呢?操作其实很简单,在单因素方差分析中,将腰围和臀围选入“因变量列表”框,将年龄分组选入“因子”框。点击“对比”,弹出对话框。在弹出的对话框中,选择“多项式”,可根据实际情况选择相应的“等级”:线性~五次。通过散点图发现年龄和腰围、臀围呈现线性关系,因此,本例选择线性。以腰围的输出结果为例,其中“组间(组合)”对应的结果即为单因素方差分析的结
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#关键词#怎么操作啊
15
***
0
谢谢,好用
58
有用
66
#trend#
28
学习了
69
学习了
83