JACC:TAVR使用和预后的种族差异
2019-05-27 xiangting MedSci原创
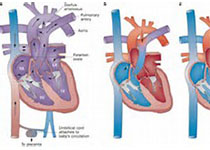
这项研究旨在评估经导管主动脉瓣置换术(TAVR)性能和预后中的种族差异。心血管疾病中的种族差异已得到了很好地描述。外科主动脉瓣置换术中观察到的种族差异是否也存在于TAVR仍然未知。在美国心脏病学会/胸外科医师协会/经导管瓣膜治疗登记中确定了2011年11月至2016年6月接受TAVR治疗的患者。描述了种族分布、风险调整后的院内发病率和按种族分层的死亡率。通过与Medicare索赔(医疗保险和医疗补
这项研究旨在评估经导管主动脉瓣置换术(TAVR)性能和预后中的种族差异。
心血管疾病中的种族差异已得到了很好地描述。外科主动脉瓣置换术中观察到的种族差异是否也存在于TAVR仍然未知。
在美国心脏病学会/胸外科医师协会/经导管瓣膜治疗登记中确定了2011年11月至2016年6月接受TAVR治疗的患者。描述了种族分布、风险调整后的院内发病率和按种族分层的死亡率。通过与Medicare索赔(医疗保险和医疗补助服务中心)进行联网评估了一部分患者的1年预后。
纳入的70,221名患者中,91.3%为白人,3.8%为黑人,3.4%为西班牙裔,1.5%为亚裔/美洲土著/太平洋岛民。与其人口比例相比,非白人患者的代表性明显不足。风险调整后,4个种族群体的院内死亡率、心肌梗死、中风、大出血、血管并发症或需要新起搏器的比率没有差异。在与Medicare联网的29,351名患者中,与白人相比,黑人和西班牙裔的1年调整死亡率相似,但亚裔/美洲土著/太平洋岛民患者的死亡率较低(调整后的风险比:0.71;95%置信区间:0.55至0.92; p=0.028)。与白人相比,黑人和西班牙裔患者的心衰住院率更高(分别为校正风险比:1.39; 95%置信区间:1.16至1.67; p<0.001;调整风险比:1.37; 95%置信区间:1.13至1.66; p=0.004)。对社会经济地位进行额外的风险调整后,这些差异仍然存在。
在美国接受TAVR的患者中,少数种族群体的代表性不足,但其调整后的30天和1年临床结局与白人相当。
原始出处:
Mohamad Alkhouli. Racial Disparities in the Utilization and Outcomes of TAVR TVT Registry Report. JACC:Cardiovascular Interventions. 27 May 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AVR#
36
#JACC#
33
#ACC#
28
#种族差异#
30