再生障碍性贫血并发慢性硬膜下血肿1例报告
2018-10-20 孙林林 付爱军 张志勇 河北联合大学学报(医学版
患者,21岁,男性。因头部外伤史2月余,突发头痛伴恶心、呕吐3天入院。入院查体:体温36.5°C,脉搏70次/min,血压130/85mmHg,呼吸18次/min。神清语利,查体合作,双侧瞳孔直径20mm光反射灵敏,颈软,无抵抗,四肢肌力V级,双侧巴氏征(+)。余查体未见明显异常。既往史:再生障碍性贫血18年,平日输注悬浮红细胞(2U、1次/3~4周)治疗,再生障碍相关贫血性心脏病史2年余。
1.病历报告
患者,21岁,男性。因头部外伤史2月余,突发头痛伴恶心、呕吐3天入院。入院查体:体温36.5°C,脉搏70次/min,血压130/85mmHg,呼吸18次/min。神清语利,查体合作,双侧瞳孔直径20mm光反射灵敏,颈软,无抵抗,四肢肌力V级,双侧巴氏征(+)。余查体未见明显异常。既往史:再生障碍性贫血18年,平日输注悬浮红细胞(2U、1次/3~4周)治疗,再生障碍相关贫血性心脏病史2年余。
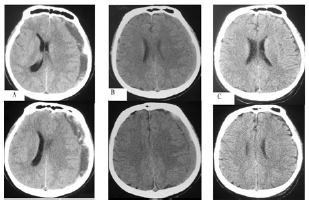
实验室检查:入院血常规提示三系减少,见表1。肝功、肾功、血脂、血糖均未见明显异常。凝血四项示:活化部分凝血活酶时间(APTT)为25s,凝血酶原时间(PT)为11s,血浆纤维蛋白原(FIB)4.42g/L,凝血酶时间(TT)为13s。颅脑CT扫描(下图A)示:左侧额颞顶部慢性硬膜下血肿(血量约70mL、最大厚度约18mm)。临床诊断:慢性硬膜下血肿;再生障碍性贫血。
2治疗经过
围手术期处理:针对患者再生障碍性贫血引起难治的三系减少,据血液系统化验给予成分输血(红细胞、血小板等)对症治疗。对症治疗前后血象变化见表1。术中及术后风险评估:患者血小板(PLT)减少可能引起出血,白细胞(WBC)减少可能感染、贫血性心脏疾病等风险。
表1 患者不同时间的血象

考虑到患者头痛症状加重,头颅CT提示具有手术指征。在全麻下行钻单孔引流术引出酱油色陈旧性不凝血。术中严密止血,静滴头孢曲松预防术后出血、感染等。术后患者头痛症状好转,术后3天无头痛症状。共住院15天痊愈出院。随访3个月良好。
患者颅脑CT扫描提示如下图:A(入院第1天):血肿高低混杂密度影,占位效应明显,左侧脑室受压明显,中线移位;B(入院第6天术前3h):血肿呈等密度影,脑沟回变浅;C(入院后第9天术后3天):血肿明显减少,脑沟回恢复。
原始出处:
孙林林, 付爱军, 张志勇,等. 再生障碍性贫血并发慢性硬膜下血肿1例报告[J]. 河北联合大学学报(医学版), 2017, 19(2):158-159.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#硬膜下#
29
#并发#
35
#慢性硬膜下血肿#
45
#血肿#
0
#硬膜下血肿#
40