J Hepatology: 白色念珠菌毒素candidalysin促进酒精相关的肝脏疾病的发展
2020-03-16 MedSci原创 MedSci原创
酒精相关性肝病是肝移植的主要指征,也是死亡的主要原因。肠道菌群的改变导致酒精相关性肝病的发病机理目前还不清楚,比如患有酒精相关性肝病的患者念珠菌的比例增加。在粪便菌群中,关于肠道念珠菌对疾
背景与目标:酒精相关性肝病是肝移植的主要指征,也是死亡的主要原因。肠道菌群的改变导致酒精相关性肝病的发病机理目前还不清楚,比如患有酒精相关性肝病的患者念珠菌的比例增加。在粪便菌群中,关于肠道念珠菌对疾病的影响知之甚少。本文中,研究人员评估了白色念珠菌及其外毒素念珠菌溶素在酒精相关性肝病中的作用。
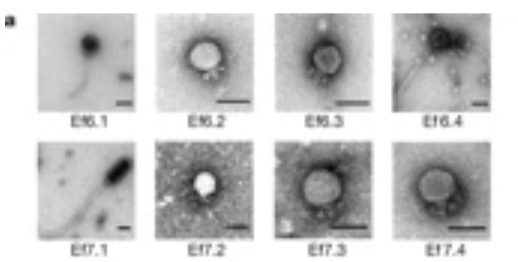
方法:研究人员对在来自对照,酒精使用障碍患者和酒精性肝炎患者的粪便样本中分析了白色念珠菌和细胞伸长程度1(ECE1)情况。将不同基因操纵的白色念珠菌菌株的小鼠接受慢性加暴饮暴食的乙醇饮食模型。最后分离小鼠原代肝细胞,并与念珠菌溶素一起孵育。
结果:在非酒精性对照,酒精使用障碍患者和酒精性肝炎患者中,携带ECE1的个体百分比分别为0%,4.76%和30.77%。念珠菌溶素加重了乙醇引起的肝病,并与小鼠死亡率增加有关。念珠菌溶素独立于骨髓来源的细胞上的β-葡聚糖受体C型凝集素结构域家族7成员A(CLEC7A),可增强乙醇诱发的肝病,念珠菌溶素不会改变肠道屏障功能。念珠菌溶素可在体外以剂量依赖性方式破坏原代肝细胞,并与酒精性肝炎患者的肝病严重程度和死亡率相关。
结论:在临床前模型中,念珠菌溶素与乙醇诱发的肝病的进展以及酒精性肝炎患者的临床结局较差有关。
原始出处:
Huikuan Chu. Et al. The Candida albicans exotoxin candidalysin promotes alcohol-associated liver disease. J Hepatology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Candidalysin#
36
#白色念珠菌#
42
#念珠菌#
35
#肝脏疾病#
52
#EPA#
31
论编刊
92