利妥昔单抗治疗结缔组织病相关间质性肺病对肺功能的影响
2022-06-27 刘少飞 MedSci原创
利妥昔单抗 (RTX) 此前曾被报道用于治疗结缔组织病相关间质性肺病 (CTD-ILD) 患者。以前没有报道过对 CTD-ILD 患者肺功能结果和相关不良反应的治疗效果大小的系统评估。
结缔组织病 (CTD) 通常与初始或随后的间质性肺病相关,通常预示着比无肺受累的 CTD 更高的发病率。虽然几乎所有 CTD 都可能与 ILD、系统性硬化症 (SSc)、特发性炎症性肌病 (IIM) 和类风湿性关节炎 (RA) 相关,但其患病率最高。放射学模式和临床表现因亚型而异,而肺功能通常以限制性通气缺陷和弥散能力降低为特征。大多数 CTD-ILD 的治疗通常涉及扩展已经针对潜在 CTD 的药物,通常包括皮质类固醇和类固醇保留剂,如环磷酰胺 (CYC)、硫唑嘌呤 (AZA) 和霉酚酸酯 (MMF)。 除硬皮病-ILD 外,由于缺乏稳健的随机对照试验 (RCT),CTD-ILD 的管理仍然是经验性或经验性的。与特发性肺纤维化 (IPF) 等其他进行性 ILD 相比,疾病亚型的异质性、不明确和可变的结果测量以及相对更好的生存率使得大型对照研究变得困难,需要持续时间更长的广泛 RCT 来区分功能或生存结果。肺功能终点通常作为治疗效果的合理标志。
利妥昔单抗 (RTX) 是一种针对人 CD20 的 B 细胞耗竭嵌合单克隆抗体,目前已被批准用于治疗淋巴瘤和 RA。先前的证据表明淋巴细胞功能的异常可能与 CTD 的发展和演变有关,因此它用于治疗其他 CTD 亚型最近引起了人们的兴趣。2008 年一项涉及 SSc-ILD 患者的初步报告 支持其在 CTD 与相关 ILD 中的特殊作用,特别是那些临床上严重或进行性肺病对常规免疫抑制无反应的患者。多个病例报告、病例系列和一项临床试验报告了利妥昔单抗在 CTD-ILD 中的积极作用,尽管其对测量肺功能的影响程度尚未总结性报道。该系统评价和荟萃分析总结了 RTX 对肺功能的综合效应大小(预测用力肺活量 (FVC%) 和一氧化碳扩散能力 (DLCO%) 的百分比),并描述了治疗 CTD-ILD 的报告安全性结果。
研究方法:
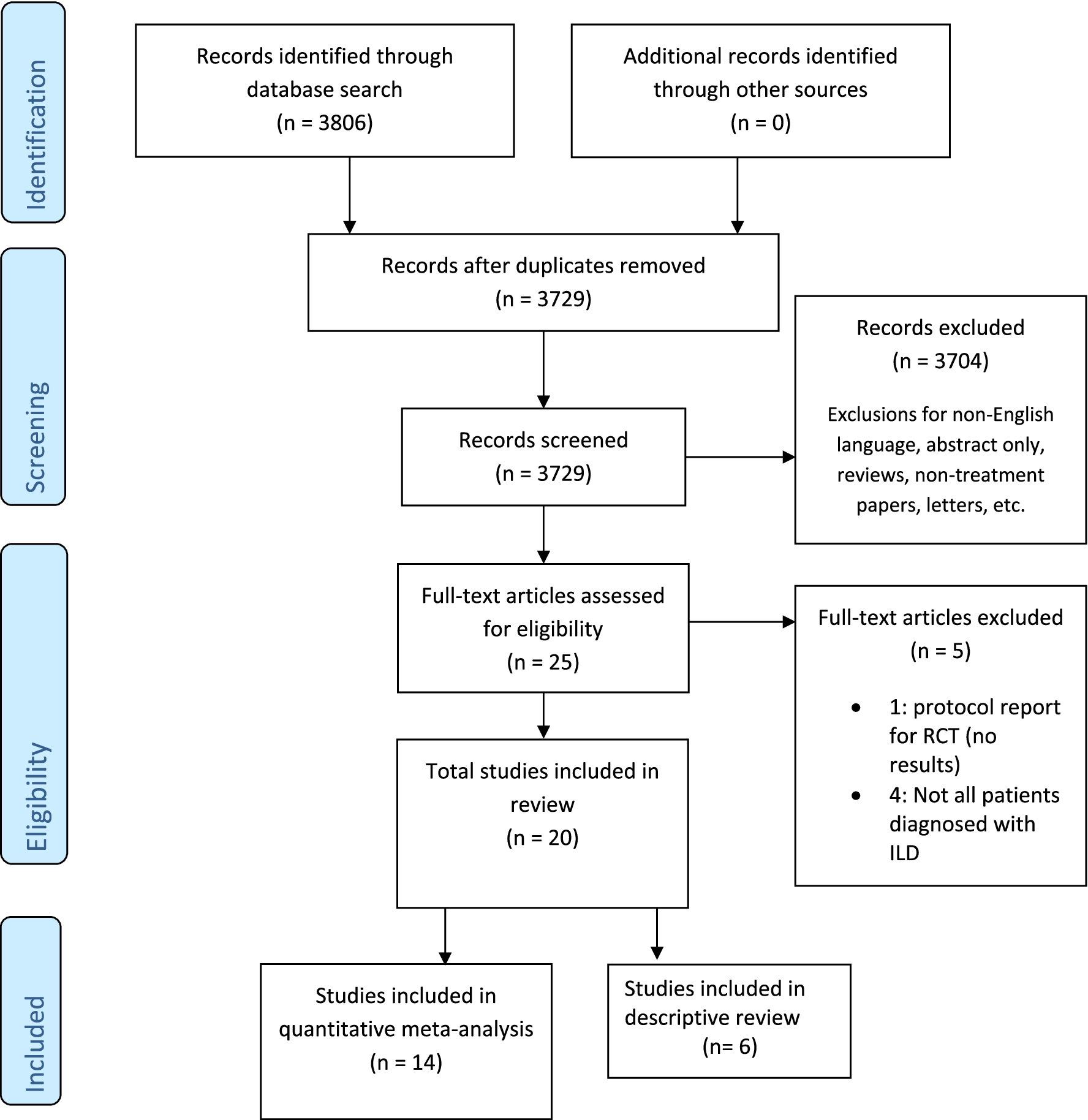
我们对来自 PubMed、Embase 和 Cochrane 图书馆的已发表报告进行了系统回顾和荟萃分析。包括包含个体肺功能数据和不良反应的随机和非随机对照试验、病例对照、队列和病例系列(有五个或更多病例)。研究终点是治疗前和治疗后预测用力肺活量百分比 (FVC %) 和一氧化碳扩散能力 (DLCO%) 的变化,以及报告的药物相关不良事件。
研究结果:
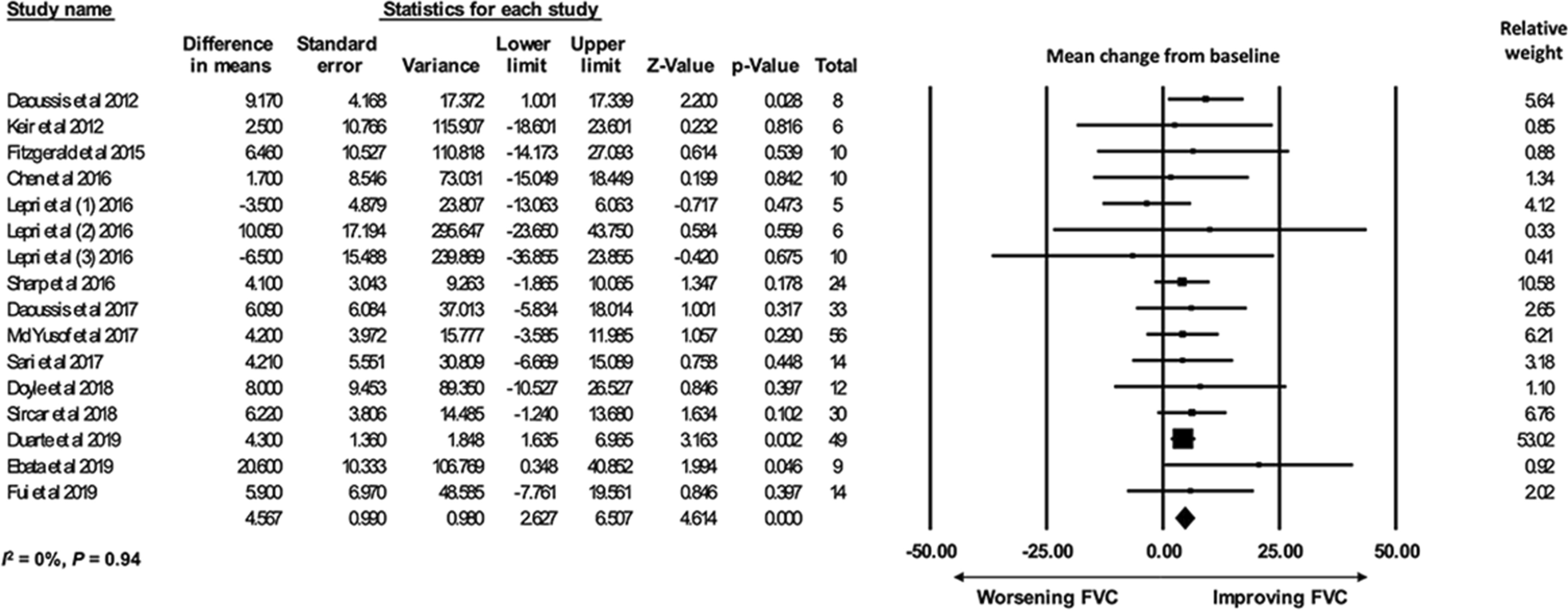
共确定了 411 名患者的 20 项研究,其中 14 项纳入肺功能荟萃分析,6 项纳入描述性综述。对治疗前和治疗后肺功能结果的随机效应荟萃分析显示 FVC% (n = 296)(平均差 (MD) 4.57%,[95% CI 2.63-6.51])和 DLCO% (n = 246) 增加) (MD 5.0% [95% CI 2.71-7.29]) RTX 治疗后。13.6% 的汇总队列报告了 RTX 治疗相关的不良反应。
研究结论:
这是第一个评估 RTX 对 CTD-ILD 患者 FVC%(MD 为 4.57%)和 DLCO%(MD 为 5.0%)的影响大小的系统评价和荟萃分析,报告的水平较低但并非不显着与药物相关的不良反应(占汇总队列的 13.6%)。每个功能终点都包含超过 240 名汇总的患者观察结果,表明 RTX 作为传统免疫抑制的辅助手段可以适度改善或稳定肺功能。目前的系统评价和荟萃分析表明,接受 RTX 治疗的 CTD-ILD 患者的肺功能(FVC% 和 DLCO%)适度稳定或改善。单独或与其他免疫抑制剂组合似乎也有相对安全的副作用。然而,缺乏随机对照试验和其他受控定量研究以及汇总数据时潜在疾病的异质性可能会对在现实世界实践中自信地使用 RTX 构成重要限制,治疗开始时要根据具体情况考虑。
参考文献:
Zhao Y, Gao Y, Petnak T, Cheungpasitporn W, Thongprayoon C, Zhang X, Moua T. Effect size of rituximab on pulmonary function in the treatment of connective-tissue disease-related interstitial lung disease: a systematic review and meta-analysis. Respir Res. 2022 Jun 21;23(1):164. doi: 10.1186/s12931-022-02082-x. PMID: 35729565.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#间质性#
41
#结缔组织#
42
#肺病#
57
#利妥昔#
42
#结缔组织病#
42