IBD: 中国炎症性肠病患者出现心血管事件风险明显增高
2022-03-06 MedSci原创 MedSci原创
根据最新研究,炎症性肠病(IBD)患者的缺血性心脏病、心血管疾病和外周动脉疾病事件的风险增加,这在55岁以下的人群中风险最高。
大量的证据表明,慢性系统性炎症是动脉粥样硬化的一个风险因素。这些发现使慢性炎症相关的动脉事件的研究取得了很大进展。因此,在各种慢性炎症性疾病中,如类风湿性关节炎、系统性红斑狼疮等,都有心脏事件风险增加的研究报道。炎症性肠病(IBD),包括克罗恩病(CD)和溃疡性结肠炎(UC),其特点是肠道的慢性炎症,以前的研究表明,IBD患者的冠心病(CHD)和缺血性心脏病(IHD)的风险增加,但是部分研究认为二者之间没有相关性,因此,本研究旨在调查中国IBD患者心脏事件的发生率和风险。

研究人员对来自中国 12 个 IBD 中心的 1,435 名 IBD 患者进行了一项回顾性队列研究。根据年龄、性别和实验室参数,将病例与来自 12 个医疗中心的 1,588 名无 IBD 的合格参与者进行了匹配,通过倾向匹配评分模型对这两组患者的心血管事件的发生率进行了统计学分析。
研究结果发现,中国 IBD 患者的缺血性心脏病 (IHD)(包括冠心病)的发病率显着高于非IBD对照组,但右束支传导阻滞和早搏的发生率低于健康对照组。IBD 患者发生 IHD 的风险明显增加,而且在 18-35 岁时达到高峰。IBD 女性患者比男性患者更容易发生 IHD。外周血中的 C 反应蛋白(CRP)水平和中性粒细胞计数与克罗恩病(CD)患者的 IHD 风险呈正相关,而血浆纤维蛋白原水平与 CD 和 CD 患者的 IHD 风险呈负相关。
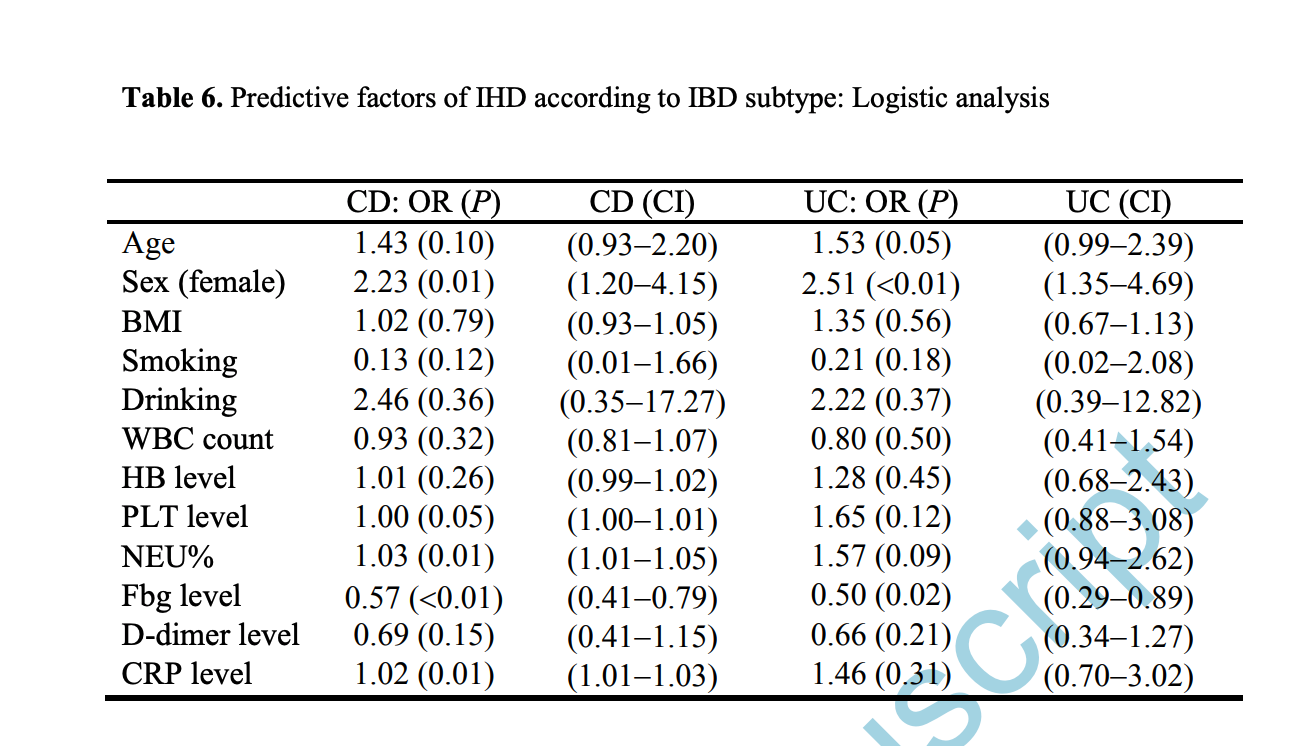
图:中国 IBD 患者的缺血性心脏病的危险因素
本项研究证实与匹配的非 IBD 受试者相比,IBD 患者发生 IHD 的风险明显增加,尤其是年轻女性 IBD 患者这样的现象更加明显。外周血中 CRP 和血浆纤维蛋白原水平以及中性粒细胞计数可能是与 IBD 患者发生 IHD 相关的潜在预测因子。该研究的结果对 IBD 患者心脏事件的管理和预防具有重要意义。
原始出处:
Leilei Fang. Et al. Risks of Cardiovascular Events in Patients with Inflammatory Bowel Disease in China: A Retrospective Multicenter Cohort Study Get access Arrow.Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管事件#
35
#炎症性肠病#与#心血管#需要有#跨学科#思维
73
学习学习
52
#IBD#
35
#心血管事件风险#
43
#炎症性#
32
#增高#
39
#增高#
40
#炎症性肠病患者#
38