右心房内的神奇“孤岛”,守护着P波?丨深度解析
2018-12-27 李学斌 何金山 医学界心血管频道
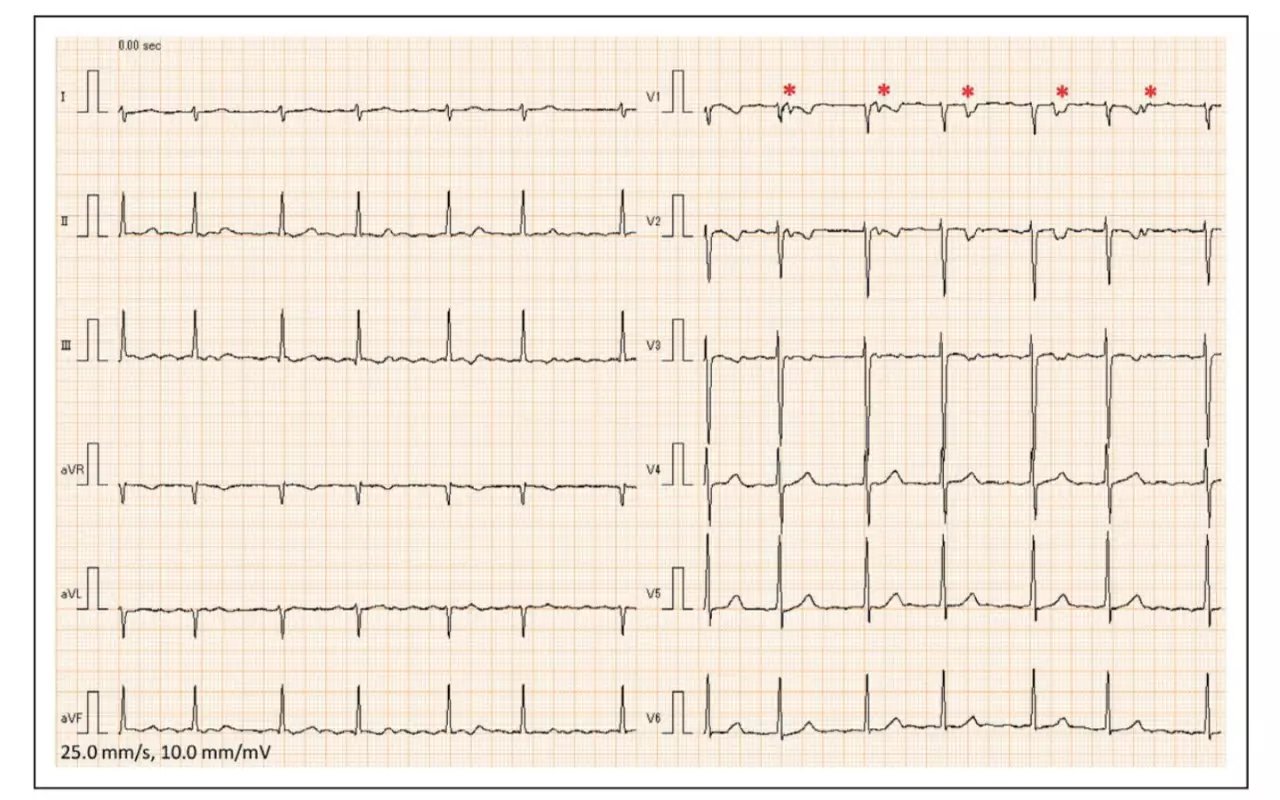
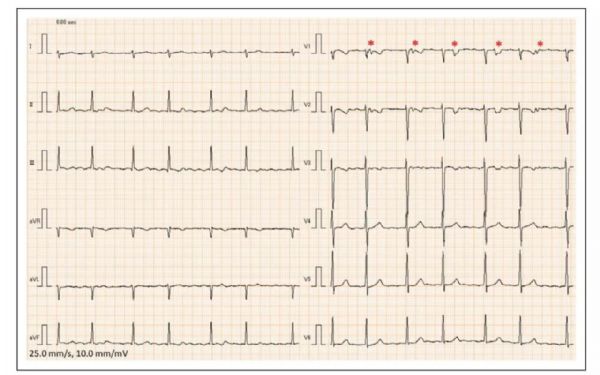
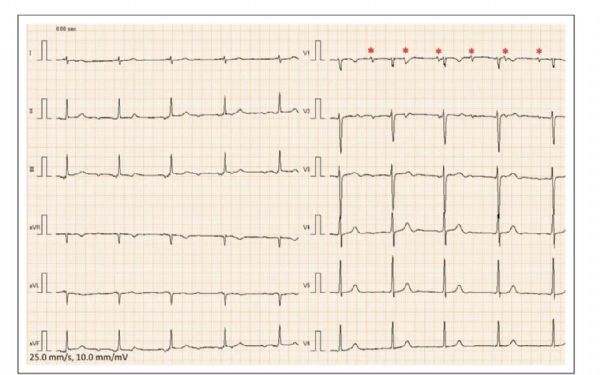
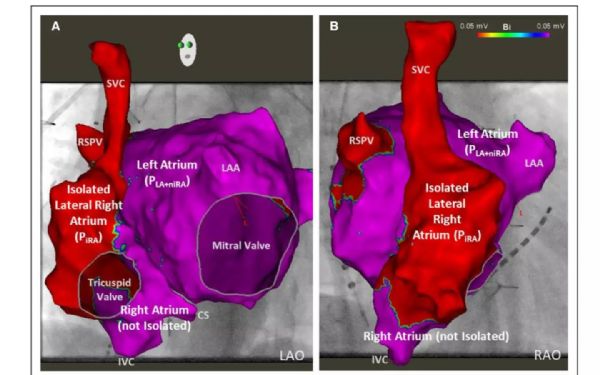
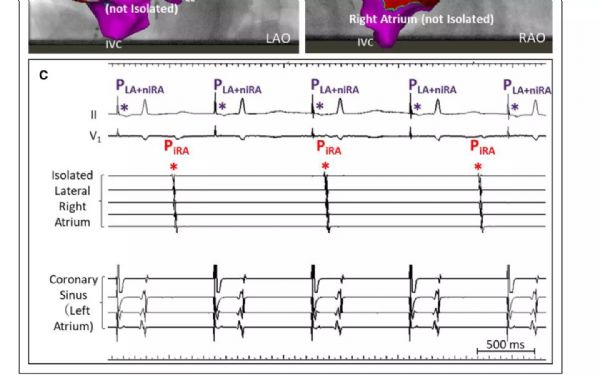
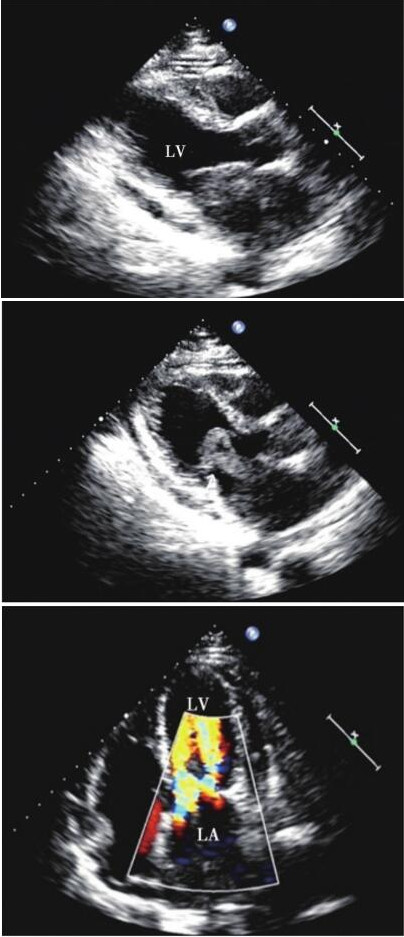
患者是46岁中年女性,既往经历过2次二尖瓣修补术,术后出现了起源自右心房的房速,进行了射频消融术,本次因出现呼吸困难和乏力就诊,就诊心电图如图1。如果只看肢体导联的话,我们可能觉得这没什么特殊的,P波消失,代之以f波,RR间期绝对不齐,这不就是房颤吗?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#解析#
32
#右心房#
63
学习了
61
#心房#
31
一个非常新鲜的病历
50