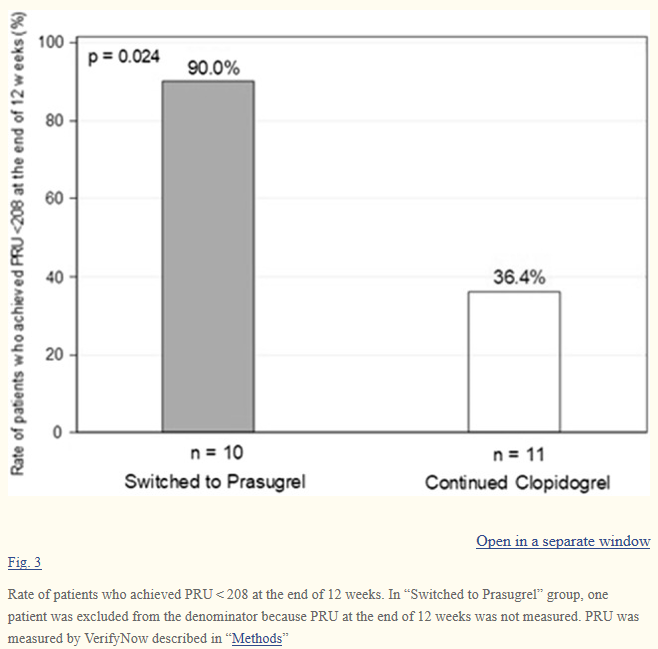
Heart Vessels:冠状动脉支架植入PCI后长期DAPT的患者,从氯吡格雷切换到普拉格雷可使PRU稳定降低
2020-11-13 MedSci原创 MedSci原创
在经皮冠状动脉介入治疗(PCI)并植入冠状动脉支架后,使用阿司匹林和P2Y12抑制剂进行双重抗血小板治疗(DAPT)。一些研究报道了PCI后从急性期到晚期,P2Y12抑制剂之间切换对血小板反应性(P2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#支架植入#
72
#冠状动脉支架#
49
#ART#
35
#DAPT#
40
#植入#
33
#HEART#
42