Nat Commun:长期服用Dasatinib和Quercetin可改善椎间盘退变
2021-09-05 haibei MedSci原创
最近,由于椎间盘退化和衰老之间的联系,研究人员探讨了抗衰老药物Dasatinib和Quercetin药物组合(D + Q)防止机体椎间盘退化的年龄依赖性进展的能力。
随着人类寿命的延长,年龄依赖性疾病的发病率和影响也在增加。在最近对50种慢性病症的全球调查中,腰痛(LBP)和颈痛分别位居生活不能自理年限的第一和第四位。虽然LBP的病因是多因素的,但椎间盘退化被认为是产生这种病理的主要因素。 重要的是,衰老会加剧椎间盘的退化和疾病的发展,因此,我们迫切需要了解椎间盘衰老的基本机制,并制定解决方案来延迟或改善年龄依赖性退化的进展。
椎间盘具有灵活性,在适应脊柱的机械负荷方面起着关键作用。这些功能特性是由三个独特的椎间盘区间相互作用实现的:中央的髓核(NP)--无血管组织,富含凝集素;周向的韧带状纤维环(AF)--主要由胶原纤维组成;以及在NP和AF的颅面和尾面接壤的软骨内板(CEP)。现在人们认识到,其中任何一个区间的功能异常都会引起其他区间的退变。
椎间盘退变的特征包括细胞外基质(ECM)的丰度和质量下降,生物力学特性的丧失,炎症介质和分解代谢过程的增加,以及细胞表型和死亡的变化。尽管患病率和疾病负担很普遍,但目前还没有针对椎间盘退变和相关病症的疾病治疗方法。

对人体组织和小鼠模型的研究表明,在椎间盘老化和退变过程中,衰老细胞的发生率增加。衰老细胞的广泛特征是细胞周期停滞,抗凋亡,并产生被称为衰老相关分泌表型(SASP)的分解代谢因子。衰老可以在各种刺激下被诱导,包括端粒损耗、致癌基因和细胞压力(如氧化性、基因毒性、细胞因子),这些刺激可以促进SASP的激活和衰老转化。
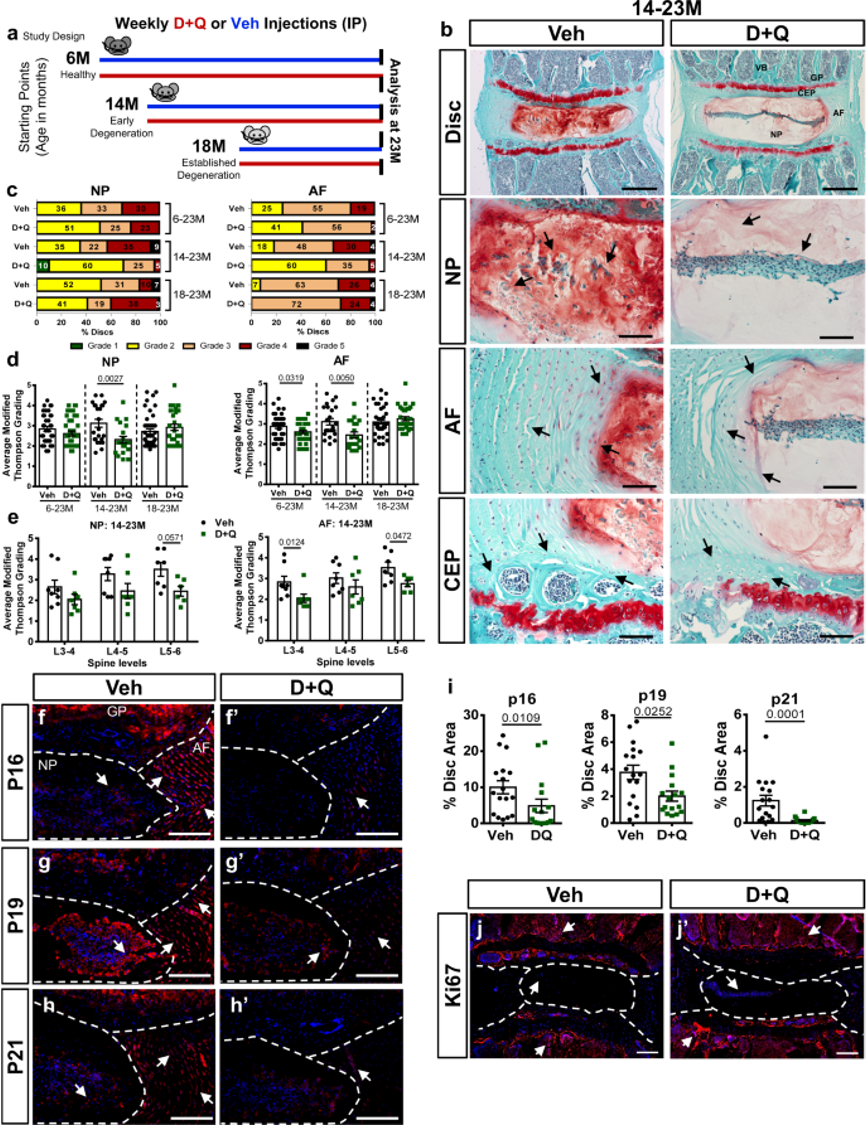
衰老药物Dasatinib和Quercetin可以减轻年龄依赖性的椎间盘退化,并降低了衰老标志物的丰度
最近,由于椎间盘退化和衰老之间的联系,研究人员探讨了抗衰老药物Dasatinib和Quercetin药物组合(D + Q)防止机体椎间盘退化的年龄依赖性进展的能力。
研究人员从6、14和18个月大的C57BL/6小鼠开始治疗,并在23个月大时对它们进行分析。有趣的是,6个月和14个月的D + Q队列显示出较低的退化发生率,而且治疗导致衰老标志物p16INK4a、p19ARF,以及SASP分子IL-6和MMP13的显著减少。此外,治疗还保留了细胞的活力、表型和基质含量。虽然转录组分析显示了治疗的盘区特异性影响,但细胞死亡和细胞因子反应途径在不同组织类型中普遍受到调制。
因此,该研究结果表明,衰老药物可能提供一个有吸引力的战略,以减轻年龄依赖性的椎间盘退化。
原始出处:
Emanuel J. Novais et al. Long-term treatment with senolytic drugs Dasatinib and Quercetin ameliorates age-dependent intervertebral disc degeneration in mice. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎间盘退变#
36
#ASA#
45
#COMMUN#
28
#Nat#
32
骨质疏松
55
~
0