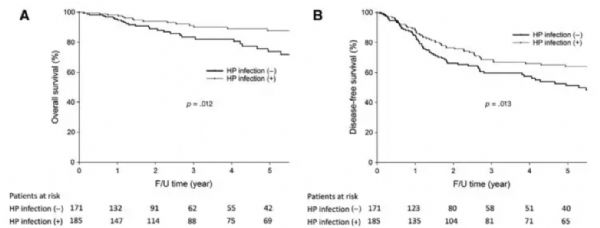
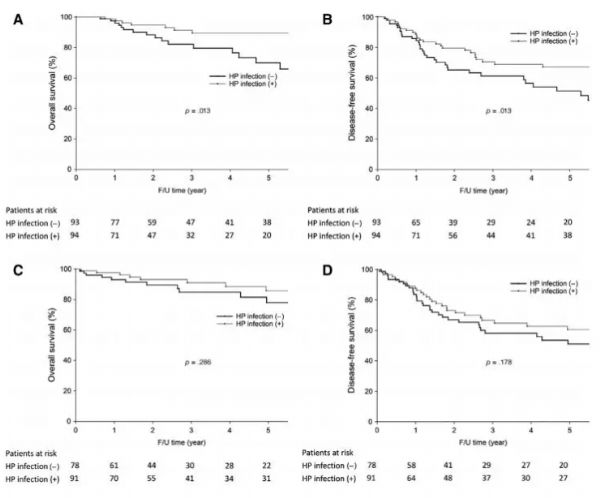
Oncologist:幽门螺杆菌感染的胃癌患者预后较非感染者更好
2019-03-10 Jelly 肿瘤资讯
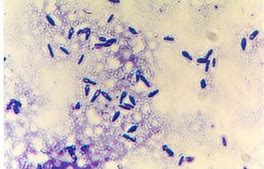
幽门螺杆菌可通过基因损伤诱导上皮细胞和肠上皮化生,使其极易发生胃癌。为了探讨幽门螺杆菌感染、基因突变和PIK3CA扩增的临床相关性及其与胃癌患者临床病理特征和预后的关系,研究者开展了该项研究,其结果发表于近期的The Oncologist杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
24
#胃癌患者#
34
#患者预后#
22
#螺杆菌#
39
#幽门螺杆菌感染#
35
#GIST#
25