Front Immunol:托珠单抗通过调控miR-146a-5p和EMMPRIN/CD147降低类风湿性关节炎血管生成
2022-01-07 医路坦克 MedSci原创
血管生成是类风湿性关节炎(RA)炎症发展的主要因素,因为血管翳的形成为浸润的免疫细胞和增殖的滑膜细胞提供了营养和氧气。
背景:血管生成是类风湿性关节炎(RA)炎症发展的主要因素,因为血管翳的形成为浸润的免疫细胞和增殖的滑膜细胞提供了营养和氧气。托西珠单抗(tocilizumab,TCZ)是一种用于类风湿关节炎(RA)患者治疗的抗IL-6受体抗体,已被证明具有抗炎作用。然而,它对血管生成的影响还没有完全阐明,调控方面的分子机制也不清楚。
方法:检测40例RA患者治疗前和治疗4个月后血清中几种促血管生成因子和抗血管生成因子的浓度,以及与RA和血管生成相关的几种microRNA分子的表达水平。此外,我们使用成纤维细胞(HT1080细胞)和单核细胞(U937细胞)的体外共培养体系来探讨TCZ的作用机制。
结果:经TCZ治疗的RA患者血清中EMMPRIN/CD147水平降低,循环miR-146a-5p和miR150-5p表达增强,血管生成能力降低,表现为EaHy926内皮细胞系形成的管状结构数量减少。体外培养HT1080成纤维细胞和U937单核细胞后,促血管生成因子EMMPRIN、VEGF和MMP-9的积聚增加,而抗血管生成因子血小板反应蛋白-1(TSP-1)的积聚和miR-146a-5p的表达水平降低。用miR-146a-5p模拟物转染HT1080细胞,可减少EMMPRIN、VEGF和MMP-9的积聚。当我们用封闭抗体中和EMMPRIN时,这些共培养上清液在功能分析中显示出迁移、增殖和管状形成的减少。
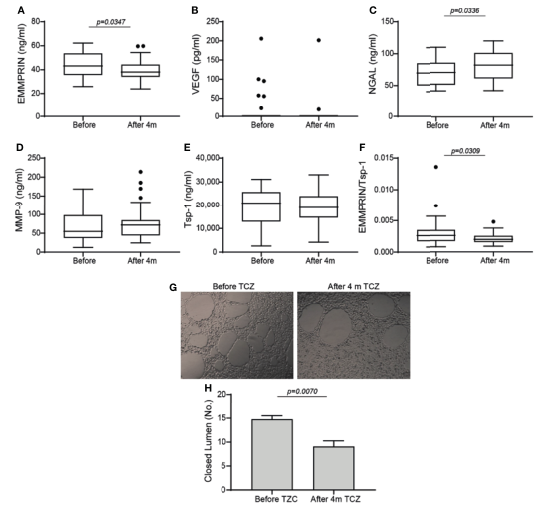
图1 RA患者接受TCZ治疗前及治疗后4个月血清中血管生成因子的变化箱形图表示在TCZ治疗开始前和4个月后RA患者的血清中血管生成介质的浓度,每个样本的重复量均确定。(A) EMMPRIN, (B) VEGF, (C) NGAL, (D) MMP-9, (E) thrombospondin1 (Tsp-1), (F) EMMPRIN和Tsp-1之间的比值作为血管生成增强的建议措施。采用非参数Mann-Whitney检验比较TCZ治疗前和4个月后每种细胞因子的浓度(n=40)。(G)管形成实验(H)封闭管腔定量,以评估血清样本对EaHy926内皮细胞的直接血管生成潜能。对选定患者的血清样本进行了3次成管试验,并使用不成对学生t检验来确定TCZ在成管试验中的作用(n=4)。
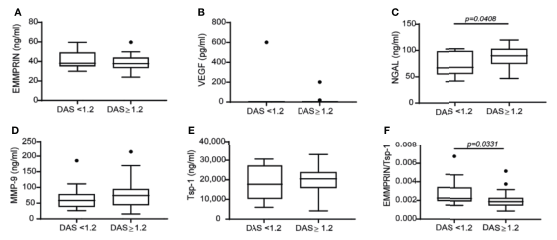
图2 除EMMPRIN/Tsp-1比值外,疾病活动评分DAS28的变化与血管生成因子浓度的差异无关。根据患者DAS28评分的变化将患者分为有应答者和无应答者,评估TCZ对血管生成因子浓度的影响。(A) EMMPRIN, (B) VEGF, (C) NGAL, (D) MMP-9, (E) Tsp-1, (F) EMMPRIN和Tsp-1之间的比值作为血管生成增强的建议措施。采用非参数Mann-Whitney检验比较TCZ治疗前和4个月后每种细胞因子的浓度(n=40)。
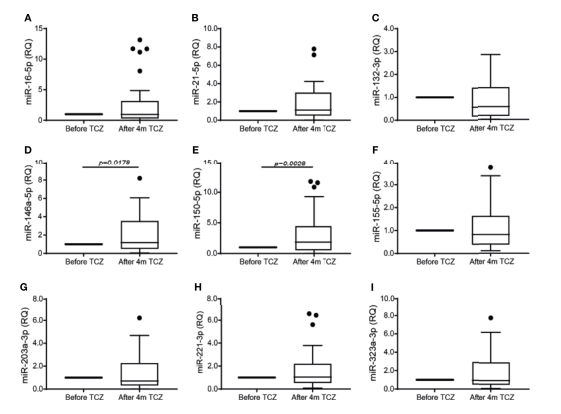
图3 TCZ治疗可增加miR-146a-5p和miR-150的血清表达。总RNA提取血清样本之前和TCZ治疗开始后的4个月和9的表达水平不同的微RNA参与血管生成和RA使用相对比较CT方法量化测定,其中每个病人担任自己的控制。miR-16-5p(一),(B) miR-21-5p, mir - 132 (C) 3 - p, mir - 146 A (D) - 5 - p, mir - 150 (E) - 5 - p (F) mir - 155 - 5 - p, mir - 203 A (G) - 3 p (H) mir - 223 - 3 - p (I) mir - 323 - A - 3 - p。采用Wilcoxon配对符号秩和检验比较TCZ治疗前和治疗后4个月各细胞因子的浓度(n=37)。
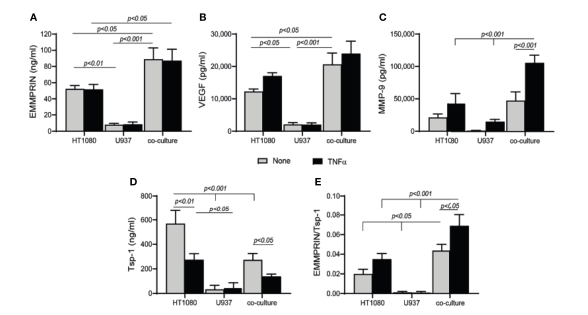
培养可促进血管生成。HT1080细胞(4x105细胞/孔,800 mL)单独培养或与U937单核细胞按1:1的比例共培养,不存在或存在TNFa (1ng/mL)。孵育48h后收集上清,采用ELISA法检测(A) EMMPRIN、(B) VEGF、(C) MMP-9和(D) Tsp-1的浓度。(E)计算每次重复的EMMPRIN/Tsp-1比值。多组比较采用双因素方差分析(ANOVA)检验,然后进行事后Bonferroni多重比较检验(n=6-7组)。
结论:我们的研究结果提示miR-146a-5p参与EMMPRIN的调控,提示TCZ通过影响EMMPRIN和miR-146a-5p影响血管生成。
原文出处:
Zisman D, Safieh M, Simanovich E,et al.Tocilizumab (TCZ) Decreases Angiogenesis in Rheumatoid Arthritis Through Its Regulatory Effect on miR-146a-5p and EMMPRIN/CD147.Front Immunol 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#托珠单抗#通过调控miR-146a-5p和EMMPRIN/CD147降低#类风湿性关节炎#
68
#CD14#
35
#miR-146a#
0
#miR#
33
太基础了,感觉看起来比较吃力
43
#关节炎#
33
#类风湿#
0
#风湿性关节炎#
44