J Clin Lipidol:在接受他汀类药物治疗的冠心病患者中,较低的LDL-C水平与较低的薄纤维帽粥样斑块发生率相关
2022-01-07 汪文慧 “心关注”公众号
近日,发表在《J Clin Lipidol》的一篇研究显示:在他汀类药物治疗的冠状动脉疾病(CAD)患者中,较低的LDL-C水平与罪犯斑块中的薄纤维帽粥样斑块(TCFAs)的较低发生率相关。
近日,发表在《J Clin Lipidol》的一篇研究显示:在他汀类药物治疗的冠状动脉疾病(CAD)患者中,较低的LDL-C水平与罪犯斑块中的薄纤维帽粥样斑块(TCFAs)的较低发生率相关。
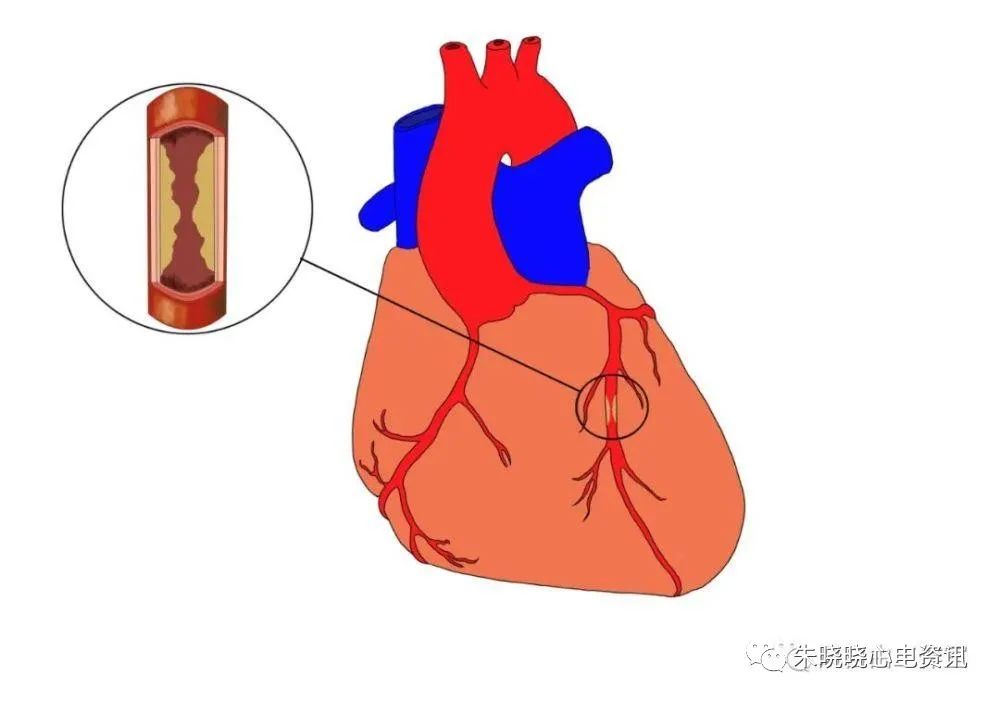
使用他汀类药物降低低密度脂蛋白胆固醇(LDL-C)水平可以减缓动脉粥样硬化斑块的进展并减少心血管事件的发生。2019年欧洲心脏病学会/欧洲动脉粥样硬化学会指南根据患者并存的危险因素推荐了<100 mg/dL、<70 mg/dL和<55 mg/dL的绝对治疗目标。为阐明他汀治疗患者的冠状动脉病变斑块特征与LDL-C水平的关系,本研究纳入685例连续接受他汀治疗的CAD患者,通过光学相干断层扫描(OCT),比较高LDL-C组(≥100 mg/dL,n=247)、中度LDL-C组(70-100 mg/dL,n=289)、低LDL-C组(70 mg/dL,n=106)和极低LDL-C组(<55 mg/dL,n=43)的罪犯斑块特征。
研究结果显示:与LDL-C水平相关的TCFA发生率显着降低(每组分别为23.1%、18.3%、9.4%、11.6%;P=0.002)。在糖化血红蛋白较低的患者中也观察到与LDL-C水平相关的较低TCFA发病率(<6.2%;P=0.003)。LDL-C<70 mg/dL(低/极低组)与缺乏TCFA独立相关(OR 0.50,95%CI 0.27-0.87;P=0.014)。
原始出处:
Hashimoto T, Minami Y, Asakura K, et al. Lower levels of low-density lipoprotein cholesterol are associated with a lower prevalence of thin-cap fibroatheroma in statin-treated patients with coronary artery disease. J Clin Lipidol. 2021 Dec 4:S1933-2874(21)00342-1. doi: 10.1016/j.jacl.2021.11.012. Epub ahead of print. PMID: 34924352.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发生率#
34
#纤维帽#
32
#他汀类药#
39
#Lipid#
53
#粥样斑块#
48
#IDO#
37
学习了
51
#斑块#
27
#LDL#
31
#冠心病患者#
44