Clin Cancer Res: Olaparib(奥拉帕利)单药维持治疗亚洲人群铂敏感复发卵巢癌的疗效:III期临床研究L-MOCA
2022-02-09 yd2015 MedSci原创
研究证实Olaparib(奥拉帕利)单药维持治疗亚洲人群铂类敏感复发卵巢癌(PSR OC)高效,且耐受良好。
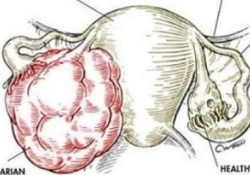
铂敏感复发(PSR)卵巢癌(OC)患者使用Olaparib(奥拉帕利)单药维持治疗较安慰剂可改善患者的PFS。但是,其在亚洲人群中的疗效尚不明确。因此,国内多中心开展了III期研究L-MOCA (NCT03534453),评估Olaparib(奥拉帕利)单药维持治疗亚洲人群铂敏感复发卵巢癌的疗效。相关研究成果发表在Clin Cancer Res杂志上。

该研究是开放标签、单臂III期研究,研究纳入中国和马来西亚的高级别上皮PSR OC患者。患者口服奥拉帕利 300 mg bid,直至疾病进展或不能耐受毒性。主要研究终点是中位PFS。
2018年至2020年,纳入了225名患者,其中224人接受了奥拉帕尼治疗。所有患者均为女性,中位年龄为54.0岁(四分位间差值为50.0 61.5),多数患者来自中国(91.5% [n=205],马来西亚8.5% [n=19])。诊断时为IV期患者31例(13.8%),III期患者152例(67.9%)。超过三分之一(35.7%)的患者曾接受过≧3种化疗,15例(6.7%)患者曾接受过贝伐单抗治疗。
半数以上(58.9%)患者无铂治疗间期>12个月,40.2% 和 0.9%患者无铂治疗间期为6-12个月和<6个月。总的来说,47.3% (n=106)的BRCAm阳性(sBRCAm 6.3 [n=14];gBRCAm 41.1% [n=92]),而BRCAwt为52.2% (n=117), 1例患者BRCA状态未知。在HRRm状态方面,HRRm 128例(57.1%),HRRwt 95例(42.4%),1例患者HRR状态未知。
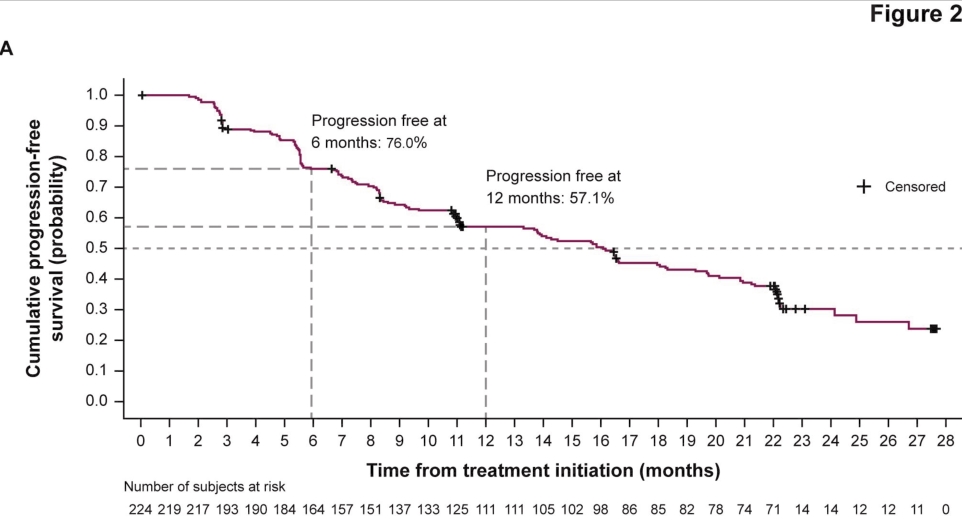
中位随访时间为15.5个月,中位PFS为16.1 个月(95% CI 13.3–18.3)。6个月和12个月无进展生存率分别为76.0 (95% CI 69.8-81.2)和57.1% (95% CI 50.2-63.5)。
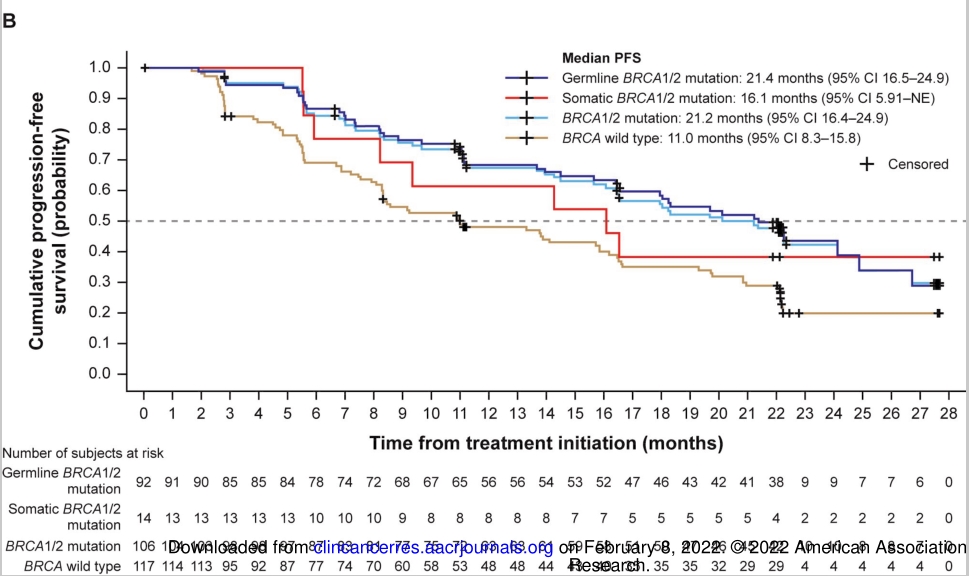
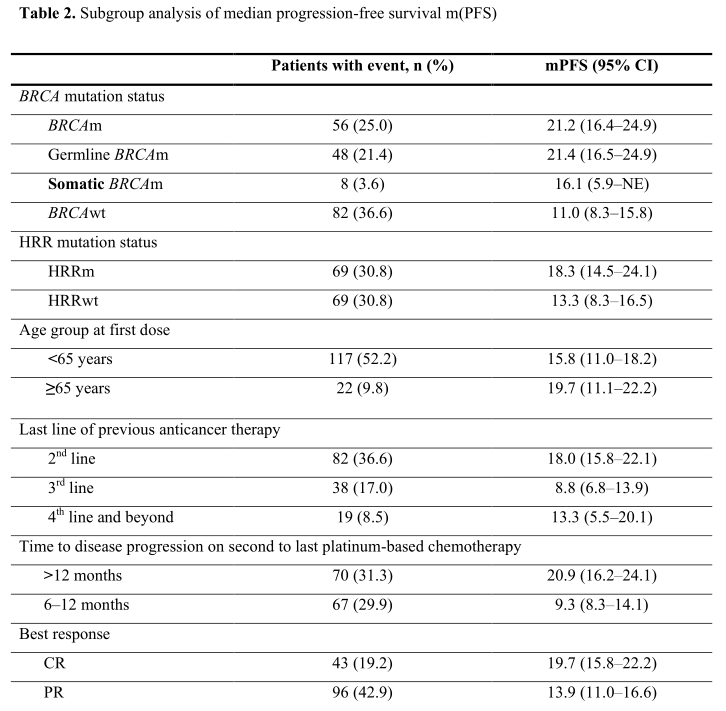
亚组分析,BRCAm和BRCAwt患者的中位PFS分别为21.2个月(95% CI 16.4-24.9)和11.0个月(95% CI 8.3-15.8)。BRCAm患者进一步分组分析,sBRCAm和gBRCAm患者的mPFS分别为16.1个月(95% CI 5.9不可评估)和21.4个月(95% CI 16.5-24.9)。HRRm患者和HRRwt患者的mPFS分别为18.3 (95% CI 14.5-24.1)和13.3个月(95% CI 8.3-16.5)。
<65岁的患者的mPFS为15.8个月(95% CI 11.0 18.2),≥65岁的患者mPFS为19.7个月(95% CI 11.1-22.2)。最后一次化疗获得CR患者的中位PFS为19.7个月(95% CI 15.8–22.2),而获得PR患者的中位PFS为13.9个月(95% CI 11.0–16.6) 。最后铂类治疗>12个月进展患者mPFS为20.9个月(95% 249 CI 16.2-24.1),而6-12个月进展患者mPFS为9.3个月(95% CI 8.3-14.1)。
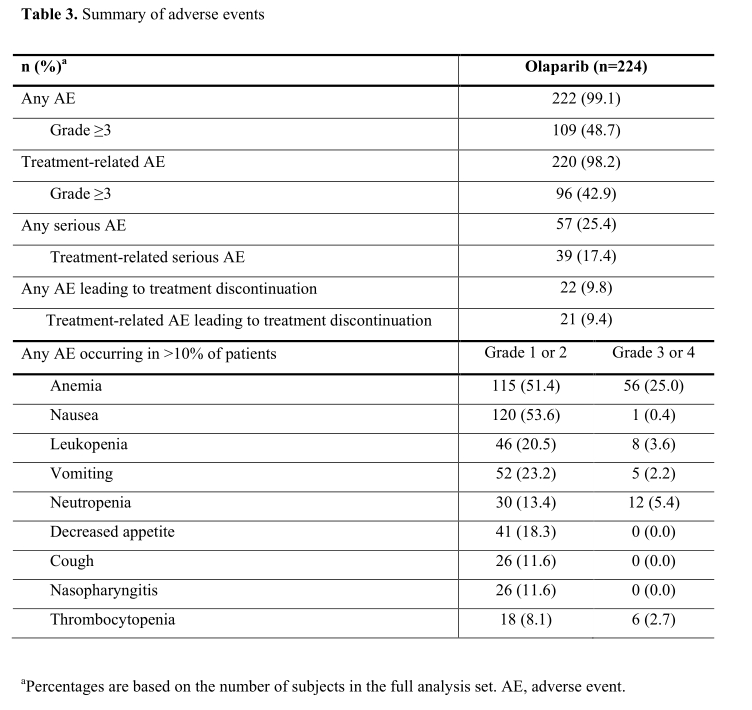
任何CTCAE分级的AEs发生率为99.1%;任何级别最常见的AEs为贫血(76.4%)、恶心(54.0%)和白细胞减少(24.1%). 48.7%的患者报告了3级或3级以上的AEs;其中,贫血(25.0%)、中性粒细胞计数下降(14.3%)和48.7%的患者报告;其中以贫血(25.0%)、中性粒细胞计数下降(14.3%)、血小板计数下降(4.9%)最为常见。严重AEs 57例(25.4%),其中治疗相关39例(17.4%)。骨髓增生异常综合征(MDS)和急性髓细胞白血病(AML) 3例(1.3%),其中2例发生在治疗期间。
综上,研究证实Olaparib(奥拉帕利)单药维持治疗亚洲人群铂类敏感复发卵巢癌(PSR OC)高效,且耐受良好。
原始出处:
Gao Q, Zhu J, Zhao W, Huang Y, An R, Zheng H, Qu P, Wang L, Zhou Q, Wang D, Lou G, Wang J, Wang K, Low J, Kong B, Rozita AM, Sen LC, Yin R, Xie X, Liu J, Sun W, Su J, Zhang C, Zang R, Ma D. Olaparib Maintenance Monotherapy in Asian Patients with Platinum-Sensitive Relapsed Ovarian Cancer: Phase III Trial (L-MOCA). Clin Cancer Res. 2022 Feb 7:clincanres.3023.2021. doi: 10.1158/1078-0432.CCR-21-3023. Epub ahead of print. PMID: 35131903.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#I期临床#
51
#III#
29
#LAP#
46
#II期临床研究#
37
#olaparib#
24
#III期临床研究#
43
#卵巢癌#
88
#铂#
23
#APA#
0
#II期临床#
36