CLIN CANCER RES:NHS-IL12治疗转移性实体瘤
2019-01-20 MedSci MedSci原创
NHS-IL12免疫细胞因子由NHS76抗体融合的两个IL12异二聚体组成。临床前研究表明,该抗体通过与游离DNA片段的组蛋白结合,将IL12靶向运输到肿瘤坏死区域,从而增强抗肿瘤活性。CLIN CANCER RES近期发表了一篇文章,研究NHS-IL12治疗晚期实体患者的最大耐受剂量(MTD)和药代动力学。
NHS-IL12免疫细胞因子由NHS76抗体融合的两个IL12异二聚体组成。临床前研究表明,该抗体通过与游离DNA片段的组蛋白结合,将IL12靶向运输到肿瘤坏死区域,从而增强抗肿瘤活性。CLIN CANCER RES近期发表了一篇文章,研究NHS-IL12治疗晚期实体患者的最大耐受剂量(MTD)和药代动力学。
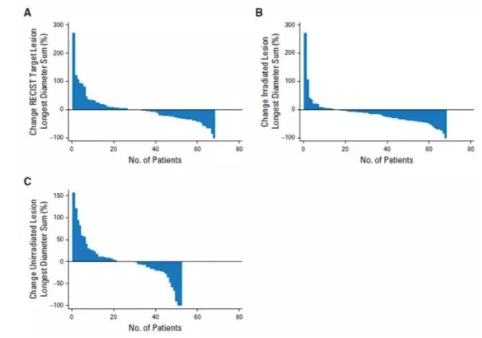
患者(n = 59)在单个递增剂量组中接受NHS-IL12皮下治疗,随后是多个递增剂量组(每4周给药n = 37)。研究结果表明,最常见的治疗相关不良事件(TRAE)包括循环淋巴细胞减少,肝转氨酶增加和流感样症状。≥3级TRAE都是暂时的,只有一个是症状性的(多汗症)。MTD为16.8μg/ kg。NHS-IL12治疗后观察到IFNγ的升高和IL10升高。在外周免疫细胞亚群中,最显着的是活化和成熟的自然杀伤(NK)细胞和NKT细胞的频率增加。T细胞受体测序分析表明,治疗后观察到T细胞受体多样性和肿瘤浸润淋巴细胞密度的增加。虽然没有观察到客观的肿瘤反应,但5名患者病情持续稳定。
原始出处:
Julius Strauss, Christopher R. Heery, et al. First-in-Human Phase I Trial of a Tumor-Targeted Cytokine (NHS-IL12) in Subjects with Metastatic Solid Tumors. CLIN CANCER RES. January 2019 doi: 10.1158/1078-0432.CCR-18-1512
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#转移性#
33
#NHS#
35
#NHS-IL12#
39