The Oncologist:中国胃癌患者不同HER2状态的治疗模式和预后:一项非干预注册研究(EVIDENCE)
2021-08-07 yd2015 MedSci原创
安全性上与曲妥珠单抗和化疗已知的安全性一致; 曲妥珠单抗治疗改善了患者预后。该研究提供了一线曲妥珠单抗联合化疗治疗中国HER2阳性mGC患者的真实世界数据。
胃癌(GC)是全球第三大癌症相关死亡原因和中国第三大常见癌症相关死亡原因。目前,治愈性手段仅限于手术切除联合围手术期或辅助化疗;对于晚期不可切除或转移性胃癌(mGC)患者,化疗是主要的治疗选择。尽管化疗可以提高患者的生存率,但由于复发和耐药率高,需要其他治疗方案。靶向治疗近年来在中国晚期胃癌的治疗中开始发挥重要作用,免疫检查点抑制剂等免疫疗法也在研究中。人表皮生长因子受体2 (HER2),在6% - 36%的GC患者中过度表达或扩增。在III期研究ToGA中,曲妥珠单抗(抗HER2单克隆抗体)可改善伴有HER2阳性的晚期胃癌患者的无进展生存期(PFS)和总生存期(OS) ,也是首个研究达到中位OS大于1年的研究。但是在现实世界中,曲妥珠单抗联合化疗治疗中国HER2阳性转移性胃癌(mGC)患者的安全性和有效性数据比较有限。因此,我国各大肿瘤中心联合开展了EVIDENCE研究,评估曲妥珠单抗联合化疗治疗中国HER2阳性转移性胃癌(mGC)患者的安全性和有效性数据。相关结果发表在The Oncologist杂志上。北京大学肿瘤医院沈琳教授为通讯作者。

EVIDENCE研究是一项前瞻性、多中心、非干预性注册研究,评估曲妥珠单抗在中国5个队列胃癌患者中的安全性和有效性,按HER2状态和曲妥珠单抗治疗进行分层。队列I (HER2阳性,曲妥珠单抗治疗)、队列II (HER2阳性,曲妥珠单抗不治疗)和队列IV (HER2阴性,曲妥珠单抗不治疗)进行有效性分析; 队列I进行曲妥珠单抗相关不良事件(AEs)分析。
OS1定义为第一次诊断复发或转移至任何原因死亡的时间;一线OS2定义为曲妥珠单抗治疗至任何原因死亡的时间;二线或三线OS2定义为一线或二线进展开始至任何原因死亡的时间。一线PFS1定义为治疗开始至疾病进展或死亡的时间。
队列I、II和IV分别包括174、113和422例患者。队列I、II和IV中接受一线化疗的患者分别有168 例[96.6%], 94例 [83.2%]和359例 [85.1%]。
在队列I、II和IV中,一线治疗的中位总生存期(OS1)分别为22.3 (95% CI,19.5–25.7)、17.2 (95% CI, 14.1–28.2)和17.4 (95% CI, 14.8–20.7)个月。排除手术患者后,中位OS1分别为19.9、15.3和12.9个月。队列I的一线、二线和三线治疗的中位OS2分别为22.1 (95% CI, 17.8-29.2)、12.0 (95% CI, 9.0 - 17.5)和10.1 (95% CI, 7.5-14.9)个月。

OS
队列I、II和IV的一线无进展生存期(PFS1)分别为8.2 (95% CI, 6.8–10.1)、6.9 (95% CI, 4.4–8.6)和6.2 (95% CI, 5.6–6.8)个月; 二线治疗的中位PFS1在队列II中最长(4.8个月vs. 3.6个月(队列I)vs 2.7个月(队列IV));同样三线治疗的中位PFS1在队列II中最长(队列II的5.4个月vs.队列I的3.2个月vs.队列IV的3.1个月)。
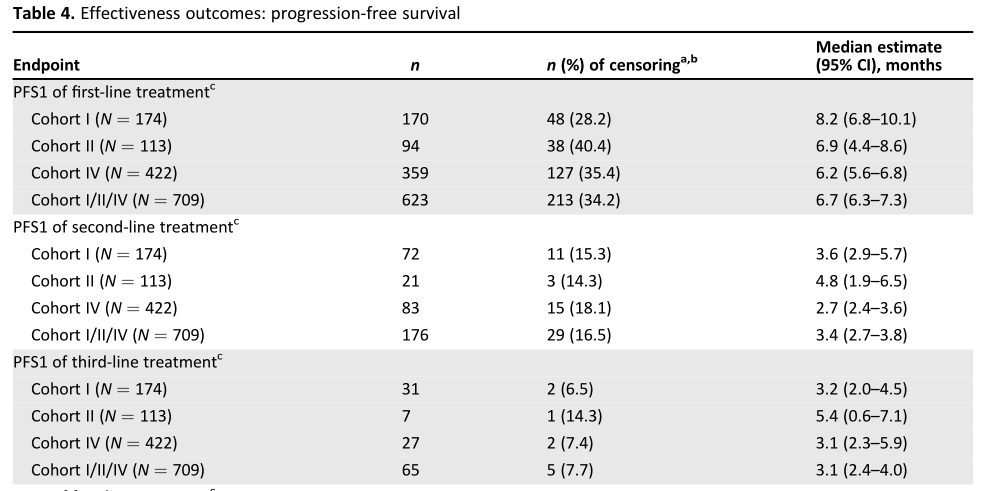
PFS
队列I、II和IV一线反应率(RR)分别为51.7%、18.4%和32.8%。所有治疗线的RR在队列I中最高。队列I中,一线、二线和三线治疗的相对危险度(RR%)分别为51.7% (95% CI, 42.4-60.9)、13.0% (95% CI, 4.9-26.3)和10.0% (95% CI, 2.8-23.7); 队列II中的分别为18.4% (95% CI, 7.7-34.3), 0%,和0%; 队列IV中分别为32.8% (95% CI, 25.9-40.3), 8.3% (95% CI, 2.3-20.0)和5.6% (95% CI, 0.7-18.7)。

RR
在倾向评分匹配的一线中位OS1(风险比[HR], 0.61)、PFS1(风险比[HR], 0.64)和RR(优势比,4.93)方面,队列I明显优于队列II。
曲妥珠单抗相关不良反应、3-5级不良反应、严重不良反应和致人死亡的不良反应分别占队列I患者的23.6%、3.4%、2.3%和0.6%。
综上,安全性上与曲妥珠单抗和化疗已知的安全性一致; 曲妥珠单抗治疗改善了患者预后。该研究提供了一线曲妥珠单抗联合化疗治疗中国HER2阳性mGC患者的真实世界数据。
原始出处:
S HUKUI Q IN , J IAFU J I , R UI -H UA X U, et al. Treatment Patterns and Outcomes in Chinese Patients with Gastric Cancer by HER2 Status: A Noninterventional Registry Study (EVIDENCE). The Oncologist 2021;26:1–14 www.TheOncologist.com
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃癌患者#
46
#注册研究#
37
#Oncol#
44
#GIST#
36
#治疗模式#
38
#注册#
29
谢谢梅斯分享这么多精彩信息
74
谈癌色变
69