JNNP:体重显著减轻后颈胸段脊髓空洞的自发消退
2021-08-17 MedSci原创 MedSci原创
脊髓空洞症或空洞是脊髓内充满液体的空洞,可产生进行性脊髓病的症状。大型症状性病变的标准护理包括直接手术干预。本文报道了一个案例,一名妇女在体重显著减轻后,颈胸腔空洞自发消退。
脊髓空洞症或空洞是脊髓内充满液体的空洞,可产生进行性脊髓病的症状。大型症状性病变的标准护理包括直接手术干预。本文报道了一个案例,一名妇女在体重显著减轻后,颈胸腔空洞自发消退。
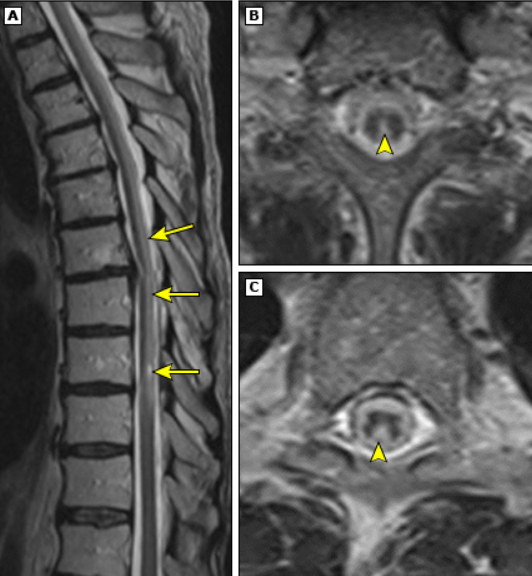
一位病态肥胖的42岁女性,体重指数(BMI)为52 kg/m2,表现为手部持续放射痛数月。患者描述了间歇性感觉异常,左手比右手感觉温度降低。她有轻微的不协调和左手无力,但在其他方面动作完好。病人否认有步态不稳或大小便失禁的问题。她既往没有外伤史,也没有特发性颅内高压(IIH)的视力丧失/症状。在没有注射对比剂的情况下,对颈椎、胸椎和腰椎进行MRI检查,发现一个巨大的颈椎和胸椎空洞,最大直径为14 mm。病人没有Chiari畸形。脑部、颈椎、胸椎和腰椎的MRI对比以及脑脊液(CSF)流动成像序列显示,无隐匿性肿瘤、蛛网膜网和颅内病变。
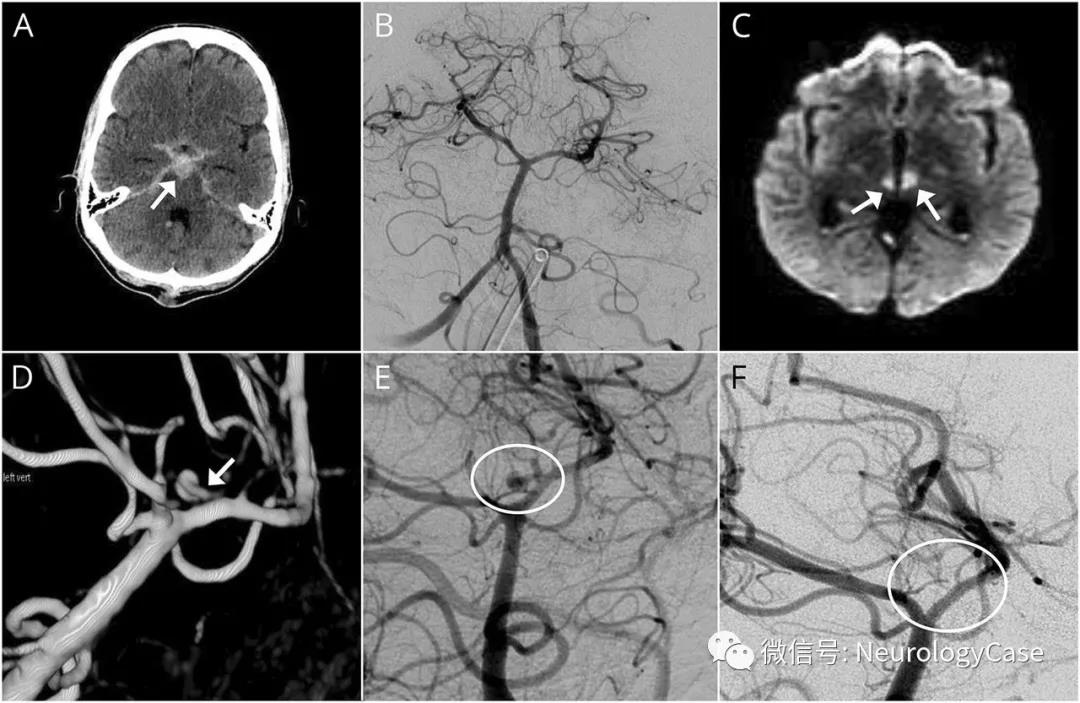
减肥前首次会诊时的MRI
考虑到患者病态肥胖和相对轻微的神经症状,患者同意进行减肥试验以降低手术风险。一位营养学家和一位减肥专家外科医生接受了转诊,并计划在一年内进行影像学随访。患者在一年内接受了腹腔镜辅助胃旁路手术。在她的下一次随访中,她减掉了约40英镑体重, 她体重指数提高到38 kg/m2。她的神经症状也有所改善,脊柱神经的MRI显示稳定的颈胸空洞。

一年后,患者的神经症状得到缓解,脊髓神经的MRI显示空洞几乎完全消退。尽管症状有所改善,但发现轻度扁桃体异位(5.2%) 嗯)。鉴于她的影像学和症状改善,医生不再建议对空洞进行神经外科治疗。
脊髓空洞症最常见于Chiari畸形,但可继发于创伤、髓内脊髓肿瘤或脊髓栓系。有人报道称,没有扁桃体异位的枕大池会导致脊髓空洞症。有趣的是,后颅窝减压术后,脊髓空洞症在这些病例中确实得到了缓解,正如Chiari I畸形所预期的那样。脊髓空洞的发生有许多可能的病理生理机制。脊髓空洞症可能会损害多种特定的病理生理学病因,导致共同的临床症状和影像学表现。对神经症状恶化的进行性空洞的外科治疗可能包括Chiari畸形减压或采用空洞-蛛网膜下腔分流术引流脊髓空洞症。
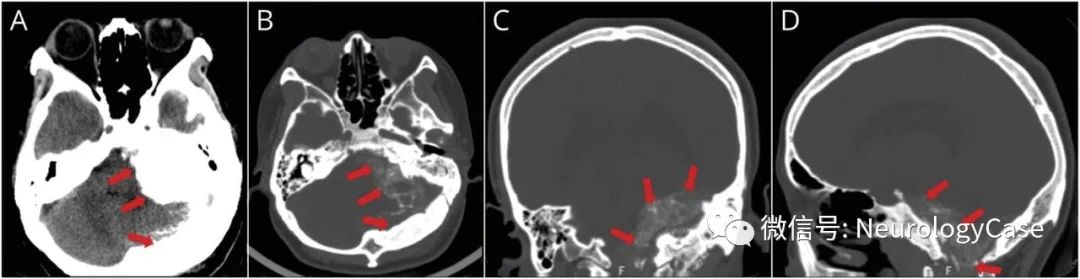
显著减肥后的MRI图像
其他人描述了罕见的脊髓空洞症自发消退(文献中仅报告了8例),尤其是与Chiari I畸形相关的病例,这是第一例报告的体重减轻后脊髓空洞症消失的病例。另一份报告描述了一名患有IIH的妇女,其颈胸空洞症是由于医源性过度通过腰腹腔分流术引起的,该分流术在怀孕后消失,据信,这是由于分娩时腹内压升高引起的分流生理学变化。事实上,正如减肥外科医生在快速减肥治疗IIH的经验中所报告的那样,脑脊液流动动力学的扰动可以随着体重的变化而解决。 Sugerman等人发现,在IIH患者中,腹压升高导致静脉压升高,进而导致脑脊液引流减少,颅内压升高。因此,随着体重减轻,脑脊液再吸收可能增加。脊髓空洞的自发消退是可能的,并且可能与患者的体重减轻是巧合的。尽管如此,对于非机械性引起的脊髓空洞,减肥可能是一种保守的治疗选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#颈胸段#
45
nice
57
nice
41
nice
42
nice
59