JAMA Netw Open:钠-葡萄糖共转运蛋白2抑制剂与2型糖尿病患者心血管转归和其他心血管疾病危险因素的相关性
2022-01-10 从医路漫漫 MedSci原创
当钠-葡萄糖共转运蛋白2抑制剂(SGLT2-IS)作为标准治疗出现时,选定人群的心血管结局尚不清楚。重要的是要了解使用SGLT2-IS在包括性别和多个年龄、种族和民族在内的选定亚组中对心血管益处

背景:当钠-葡萄糖共转运蛋白2抑制剂(SGLT2-IS)作为标准治疗出现时,选定人群的心血管结局尚不清楚。重要的是要了解使用SGLT2-IS在包括性别和多个年龄、种族和民族在内的选定亚组中对心血管益处的大小。
目的:利用从随机临床试验中获得的数据,在较大样本量的预先指定组中,评估SGLT2-IS的使用与心血管益处之间的关系。
数据来源:搜索电子数据库PubMed、Google Scholar、Web of Science和Cochrane,从最初到2021年1月10日,通过会议论文和会议演示文稿、ClinicalTrials.gov和已发表研究的参考列表确定其他研究。
资料选择:本研究纳入了安慰剂对照的随机临床试验,这些试验的参与者有动脉粥样硬化性心血管疾病(ASCVD)或ASCVD、糖尿病或心力衰竭的危险因素,并报告了主要结果。多中心观察性和非观察性研究以及那些有不同兴趣结果的研究被排除在外。
数据提取与综合:医学主题搜索词包括SGLT2-I和不同组合的多种心血管结果。这项研究遵循系统回顾和荟萃分析(PRISMA)报告指南的首选报告项目。使用Mantel-Haenszel方程和随机效应模型对所有结果进行分析。
主要结果和测量:使用SGLT2-I的6个疗效结果(心血管死亡和心力衰竭住院作为主要结果,主要心血管不良事件,心力衰竭、心血管死亡、急性心肌梗死和全因死亡作为次要结果)进行评估。对心血管死亡或HHF的主要结局进行亚组分析。使用优势比(OR)和95%的顺应性来比较两种干预措施。
结果:共纳入10项研究,71553名参与者,其中39053人接受SGLT2-IS,在报道这些数据的研究中,28809名男性和15655名女性(平均年龄65.2[范围,61.9-70.0]岁)。种族和民族是在最初的试验中定义的,在本分析中被归类为亚洲人、黑人或其他人(6900名参与者)和白人(26646名参与者)(“其他”类别没有统一指定)。以年龄计算,65岁以下的有16793人,65岁或以上的有17087人。在平均2.3(0.8-4.2)年的随访中,SGLT2-I组倾向于减少主要结果(3165/39 053[8.10%]vs 3756/32 500[11.56%];OR,0.67[95%CI,0.55-0.80];P<0.001)。与安慰剂组相比,急性心肌梗死的发生率没有差异(26931人中的1256人[4.66%]对20373人中的958人[4.70%];OR,0.95[95%CI,0.87-1.03];P=0.22)。亚组分析倾向于将SGLT2-I用于性别、年龄组、种族和民族组的主要结果。
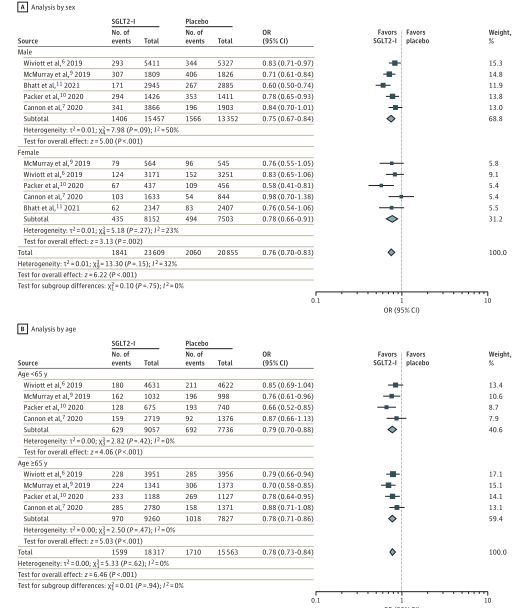
按性别和年龄划分的亚组分析
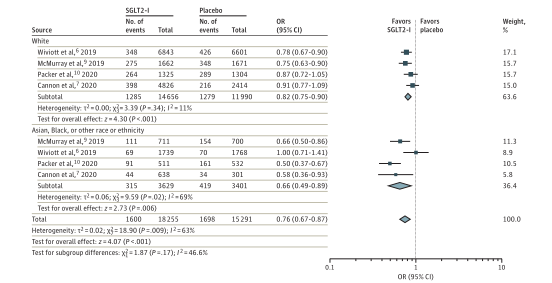
按种族划分的亚群分析
结论:这项荟萃分析支持SGLT2-IS已成为改善选定患者心血管发病率和死亡率的有效药物类别。钠-葡萄糖共转运蛋白2抑制剂与降低急性心肌梗死的风险无关。未来的长期前瞻性研究是必要的,以了解其对心血管的长期益处。
原文出处:
Bhattarai M, Salih M, Regmi M,et al.Association of Sodium-Glucose Cotransporter 2 Inhibitors With Cardiovascular Outcomes in Patients With Type 2 Diabetes and Other Risk Factors for Cardiovascular Disease: A Meta-analysis.JAMA Netw Open 2022 Jan 04;5(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
42
#抑制剂#
25
#2抑制剂#
50
#心血管疾病危险因素#
32
#PE#
37
#转运#
25
#相关性#
22
对
41
学习了
45
#2型糖尿病患者#
24