目前,中风是我国国民的第一位死亡病因。
覆盖50万名成年人的中国慢病前瞻性研究9年随访结果表明,我国患者首次出现中风发作5年内,中风复发或死亡的风险均很高。
在首次中风发作后28天时仍存活的患者中,5年时四成再次出现中风,17%死亡。
研究者指出,尽管我国的脑卒中治疗取得了明显进展,但患者的短期和长期预后仍很差,因此亟需进一步改善脑卒中二级预防,以降低复发和死亡风险。
同时,脑卒中一级预防也仍需加强,主要是生活方式调节。
该研究显示,在我国首次出现中风发作的患者中,脑出血患者的28天死亡率高达47%,其中蛛网膜下腔出血患者的28天死亡率为19%;待分类中风患者的28天死亡率为24%,缺血性中风患者中为3%。
城乡差距非常明显,以蛛网膜下腔出血为著,城市和农村患者的28天死亡率分别为32%和52%。
在我国首次出现中风发作、28天时仍存活的患者中,5年时中风复发率高达41%;其中,缺血性中风、脑出血、蛛网膜下腔出血、待分类中风患者的复发率分别为41%、44%、22%、40%。
在所有首次中风发作28天时存活的患者中,5年死亡率为17%;脑出血患者5年死亡率最高,为28%,其中蛛网膜下腔出血患者5年死亡率为16%;缺血性中风、待分类中风患者的5年死亡率分别为16%和15%。
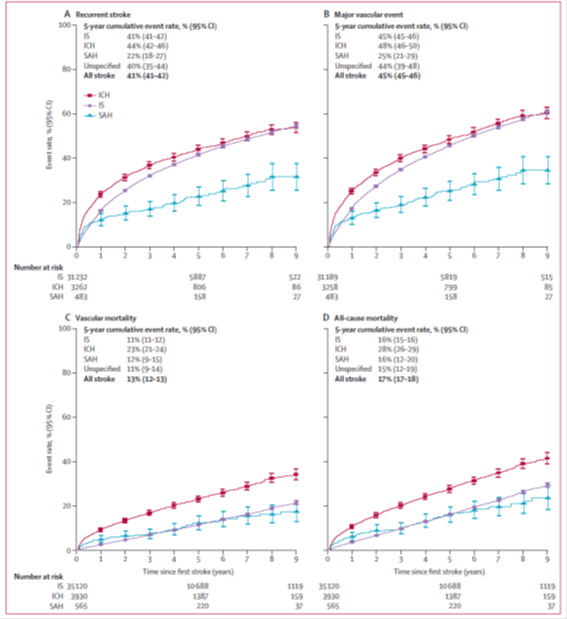
不同类型中风患者首次发作28天后中风复发(A)、主要血管事件(B)、血管性死亡(C)、全因死亡(D)的估算累积发生率
在首次发生缺血性中风的患者中,91%的中风复发类型仍未缺血性中风。
在首次出现脑出血的患者中,56%的中风复发类型仍为脑出血,但有41%为缺血性中风。
中国慢病前瞻性研究共纳入512 715名35~74岁的成年人,其中489 586人基线无缺血性心脏病或中风,接受随访9年。
研究期间,45 732人(9.3%)首次出现中风发作,其中缺血性中风、脑出血、蛛网膜下腔出血、待分类中风分别占80%、16%、2%、2%。
中风患者和未出现中风者的平均年龄分别为59.3岁和50.8岁。
原始出处:
Yiping Chen,et al.Mortality and recurrent vascular events after first incident stroke: a 9-year community-based study of 0.5 million Chinese adults. The Lancet Global Health, 2020, 8(40): PE580-E590.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#前瞻性研究#
29
#Lancet#
26
#前瞻性#
24
#中风患者#
30
中风是俗称,应该称为缺血性卒中吧
58