Neurology:病例:继发于硬脊膜动静脉瘘的脊髓瘘
2018-08-02 zyx整理 神经科病例撷英拾粹
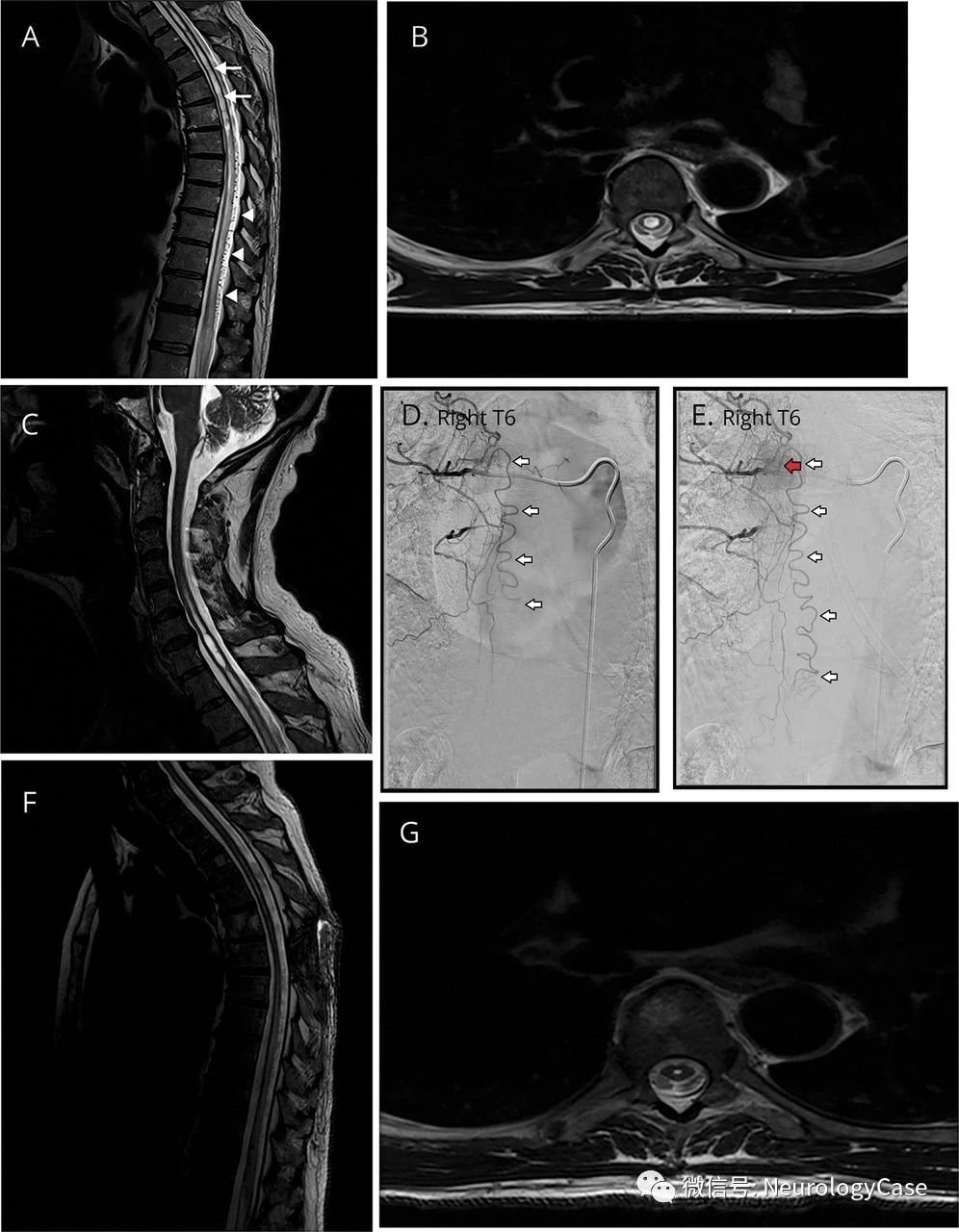
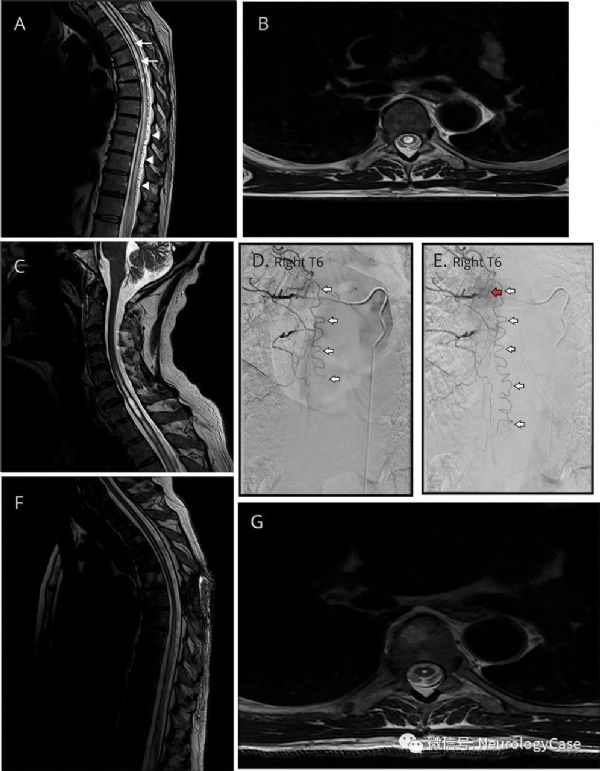
60岁男性,表现为进行性下肢无力,麻木,尿潴留以及慢性便秘伴严重截瘫的叠加发作2年。MRI提示颈胸髓瘘伴流空信号(图)。脊髓血管造影可见I型硬脊膜动静脉瘘(SDAVF),行外科手术结扎治疗。患者临床症状明显改善,脊髓瘘消失。
60岁男性,表现为进行性下肢无力,麻木,尿潴留以及慢性便秘伴严重截瘫的叠加发作2年。MRI提示颈胸髓瘘伴流空信号(图)。脊髓血管造影可见I型硬脊膜动静脉瘘(SDAVF),行外科手术结扎治疗。患者临床症状明显改善,脊髓瘘消失。先前有另一个与SDAVF相关脊髓瘘的病例报告,结局类似。胸段SDAVF常见于男性,在60-70岁时出现,运动时腿部无力加重,可能是脊髓瘘一可治病因。
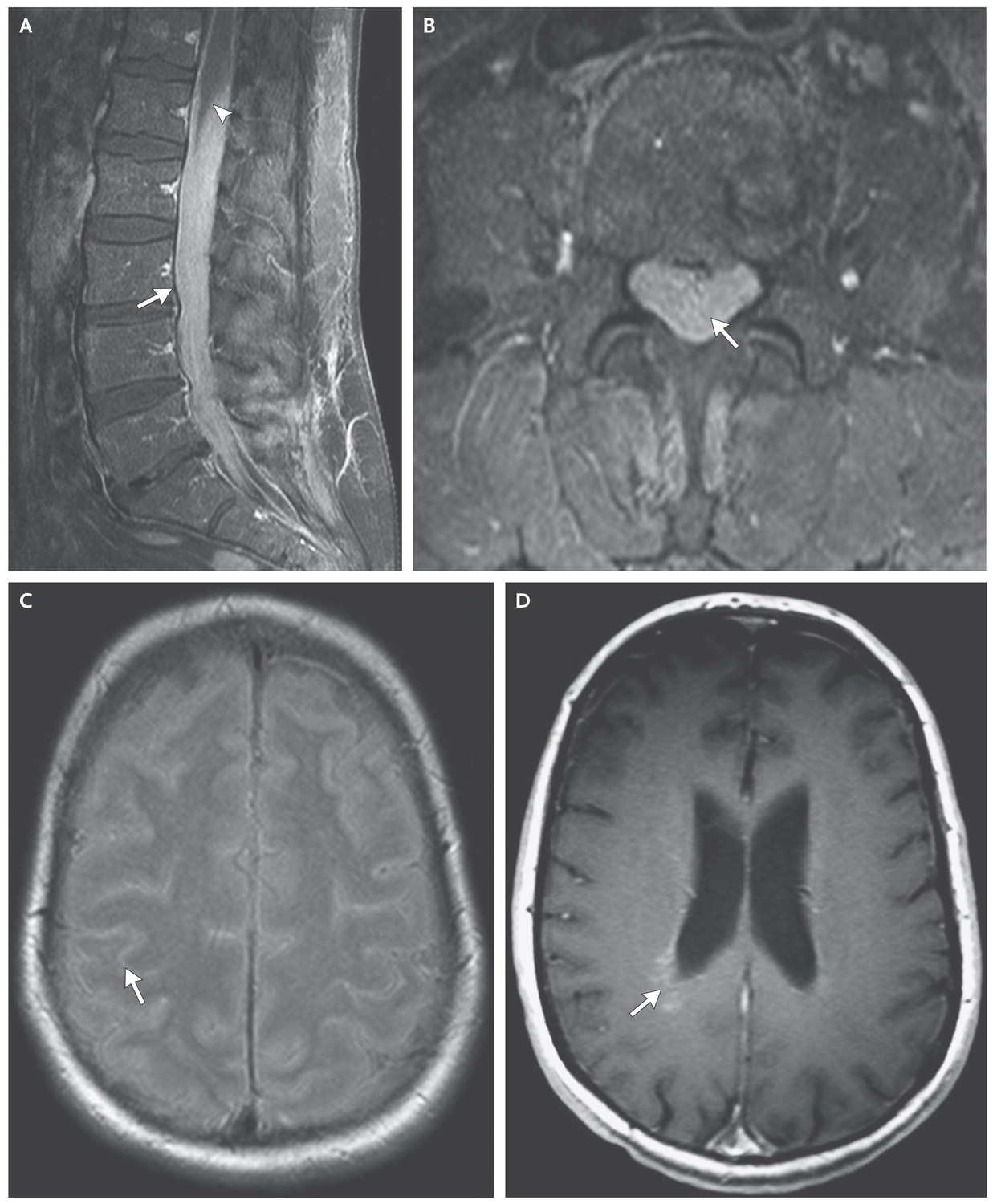
(图:A:矢状位MRI可见从胸髓延伸至圆锥的T2高信号;大部分与脊髓肿胀和水肿有关;此外,可注意到瘘[箭]伴中央管扩张,从下颈髓延伸至大约T8水平,其后中央管轻微突出;T6至圆锥可见许多背侧硬膜外匐行流空信号[箭头];B:横断面T2WI可见T4水平的瘘;C:头颅矢状位T2WI可见瘘从C2-3下方延伸至胸髓; 以C7水平最为严重;小脑扁桃体未见移位;D:早期血管造影可见迂曲的引流静脉[箭头];E:晚期血管造影可见右侧T6椎弓根右下方的硬脊膜动静脉瘘[红箭],由T6肋间动脉供血;伴一条迂曲的引流静脉[白箭]下行;F-G:矢状位和横断面T2WI提示在瘘管结扎后8周脊髓瘘消失)
原始出处:Zaed I1, Pinto MV1, Mauermann ML1, Lanzino G2. Teaching NeuroImages: Spinal cord syrinx secondary to a spinal dural arteriovenous fistula. Neurology. 2018 Jul 17;91(3):e295-e296.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Neurol#
22
#继发#
29
#静脉#
30
#动静脉瘘#
41
#硬脊膜#
33