Ann Thorac Surg:积极治疗早期肺癌可提高生存率
2018-01-05 佚名 肿瘤免疫细胞治疗资讯
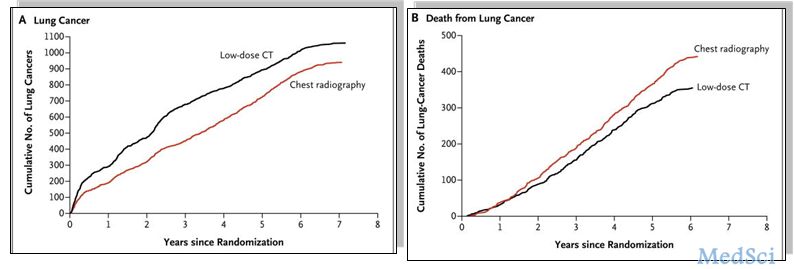
加利福尼亚大学圣地亚哥分校医学院的研究人员表示,哪种方法更能改善生存方面的优越性还不清楚。以前的研究试图比较每个过程的病人结局,但结果却不尽相同。在这项研究中,研究人员进行了一种对早期肺癌的最大和最详细的分析。在4069例患者的研究中,多数行肺叶切除,16%例亚肺叶切除,11%接受SBRT。研究人员发现,治疗之后的五年,在切除组有23%患者死亡,采用放射治疗的患者45%死亡,亚肺叶切除患者的死亡率
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#THORAC#
28
#早期肺癌#
37
同意比调查研究!受益匪浅!
62
好知识.值得学习
56
好知识值得学习
56
好知识.值得学习
46
好知识.值得学习
63
好知识!值得学习
21
好知识.值得学习
18
好知识.值得学习
24