JCEM:细菌脓毒症和COVID-19患者TSH和甲状腺激素与淋巴细胞减少之间的关系
2021-03-23 MedSci原创 MedSci原创
在细菌脓毒症和COVID-19等严重感染患者中,甲状腺功能异常与淋巴细胞减少相关,但未来的研究需要确定是否存在因果关系。
淋巴细胞减少是细菌性脓毒症和COVID-19患者免疫功能障碍的一个关键特征,并与患者不良临床结局相关,但其原因很大程度上处于未知。重症患者可能出现甲状腺功能异常,即所谓的非甲状腺疾病综合征(NTIS),一些研究已经将TSH和甲状腺激素甲状腺素(T4)和三碘甲状腺原氨酸(T3)与淋巴细胞群的稳态调节和功能联系起来。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在评估严重感染患者甲状腺功能异常与淋巴细胞减少之间的相关性。
研究人员回顾性地分析两个独立的住院研究人群:细菌脓毒症(224例)和COVID-19患者(161例)的绝对淋巴细胞计数、循环TSH、T4、游离T4 (FT4)、T3、白蛋白和炎症生物标志物。研究人员对严重淋巴细胞减少和淋巴细胞计数正常的患者进行亚组分析。
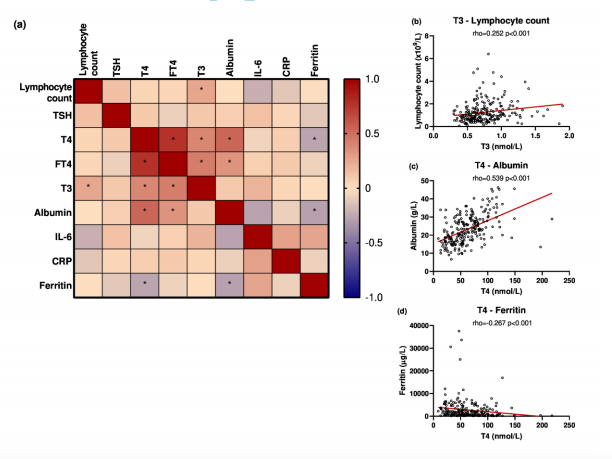
在细菌脓毒症患者中,只有T3与淋巴细胞计数显著相关(rho=0.252),重度淋巴细胞减少患者淋巴细胞计数低于非淋巴细胞减少患者(n=56/组)。17例严重淋巴细胞减少的COVID-19患者血浆TSH、T4、FT4和T3浓度明显低于无淋巴细胞减少的COVID-19患者(n=18),炎症标志物白细胞介素-6、c反应蛋白和铁蛋白显著升高。值得注意的是,随访1周后,多数(12/15)COVID-19患者淋巴细胞数量定量恢复,但TSH和甲状腺激素仍以紊乱为主。
由此可见,在细菌脓毒症和COVID-19等严重感染患者中,甲状腺功能异常与淋巴细胞减少相关,但未来的研究需要确定是否存在因果关系。
原始出处:
Inge Grondman.et al.The association of TSH and thyroid hormones with lymphopenia in bacterial sepsis and COVID-19.JCEM.2021.https://doi.org/10.1210/clinem/dgab148
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCE#
31
学习了
54
#JCEM#
30
学习啦
66
#COVID-19患者#
34
#淋巴细胞#
31
#TSH#
42
学习了
66
学习了
74
学习学习
73