10多年前波诡云谲的SARS已经离我们远去,但遗留下来的问题不少,骨坏死就是问题之一,据粗略统计,在北京感染SARS的医务人员中,有1/3~1/2出现骨坏死。在生活中您也许听说过某人因为长期酗酒,结果股骨头坏死,做手术换了金属关节。
“骨头也能坏死,还能走路吗?”
您是不是觉得特别疑惑和不解。
到底什么是骨坏死,它会带来什么后果?
其实这种骨坏死多表现为股骨头坏死,也有人出现踝关节、膝关节、肩关节坏死。骨坏死因早期表现不明显,致使误诊、漏诊率相当高。骨坏死一旦发生,如果未经治疗,至少有80%的患者将遵循“坏死-塌陷-骨性关节炎”的发展规律,在伴随关节疼痛的同时,逐渐导致关节活动及行走功能部分或完全丧失,可见危害十分严重。那我们就来说说什么是骨坏死?怎么才能早期发现?
一、什么是骨坏死?
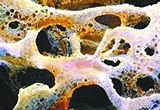
骨坏死又称无菌性骨坏死或缺血性骨坏死,指骨的有活力成分(包括骨细胞、骨髓造血细胞及脂肪细胞)死亡所引起的病理过程。常见于股骨头、肱骨头、股骨髁、胫骨近端及足、踝、腕部骨组织,其中股骨头最易遭到侵犯,常双侧受累。故本文主要以股骨头无菌性坏死为例进行讨论。
二、如何才能早期发现股骨头坏死呢?
1.注意与股骨头坏死发病有关的敏感因素
创伤(特别是股骨颈骨折),减压病,放射损伤,Gaucher病,血红蛋白病、类固醇皮质激素,酒精中毒等。创伤、酒精和激素是临床最常见的三种原因。
2.临床表现
股骨头坏死早期症状较少甚至无表现,疼痛常常是股骨头坏死最早的症状,通常是慢性隐痛,但疼痛症状并非长期持续,经休息或减少活动,症状往往减轻或自行消失。有些患者仅在髋部、臀部及大腿后侧感到牵掣不适,痛处可有不同程度的肿胀和关节功能障碍。这些轻微的症状常常为患者所忽略。加上这些症状并非特异性,而接诊医生又缺乏经验,或就诊医院的设备条件等有限,常常将该病漏诊或误诊为“风湿”、“腰椎间盘突出症”等病。
此疼痛可发生于X线片阳性发现之前或之后。疼痛反复发作,特别是减轻不明显后提示病情加重。股骨头坏死患者中后期可出现跛行,患肢肌肉废用性萎缩。患髋部各方向活动受限,以内旋和外展受限为主,腹股沟中点压痛,肌肉萎缩以股四头肌为显着,可出现易疲劳,行走乏力。
3.辅助检查
①X线检查
X线是目前诊断骨坏死最常用的一种方法,也是观察骨坏死治疗效果的一种常用有效方法,具有简单、直观、方便、经济的特点。但发现时间滞后,不利于早期检查。早期,X线片上常无阳性表现。中期,可见明显的坏死区,骨密度减低和增高同时出现,“新月征”阳性,可见骨区塌陷。后期,软骨下骨板及关节面塌陷,骨轮廓改变,阶梯状不连续,骨压缩加重,同时髋臼关节面也受损,关节间隙狭窄,骨赘形成。
②同位素扫描
对缺血性骨坏死诊断敏感性达80%,比常规X线检查更早地反映病变情况。
③CT检查
CT具有分辨力高和精确对比的特点,能对骨坏死作出早于X线片的诊断,敏感性90%以上,特异性强。
骨坏死的CT表现:早期呈正常或星状结构变形,负重骨小梁增粗紊乱,可见局限性囊样变疏松区及散在的斑点状钙化区;中晚期表现为骨轮廓变形,碎裂及髓腔硬化等。
④MRI检查
MRI检查为目前公认的诊断骨坏死最为敏感的方法,具有理想地显示骨骼系统形态、结构和功能的特点,明显优于X线、CT检查和同位素扫描,时候对有诱发因素的患者早期排除病变。
⑤其他
如骨的血液动力学检查、动脉造影检查、穿刺活检等对骨坏死的早期诊断常有帮助。 其血液检查常无特异性,为了鉴别诊断,可作血的碱性磷酸酶、类风湿因子、血沉等检验。
4.我们的建议
注意相关的发病诱因如长期酗酒、应用激素,有临床症状的表现如髋部不明原因反复疼痛,跛行,休息无缓解等,毋须紧张,要定期行影像学检查,及时咨询专家,是发现和排除骨坏死的最佳方法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#骨坏死#
32
#X线#
26
#坏死#
15
好文章,谢谢
39
很好,谢谢分享,学习了
41
好文章学习了
34