Diabetes:糖尿病人嗅觉减退?可能是这种病的前兆!
2018-05-04 黄晶 医师报
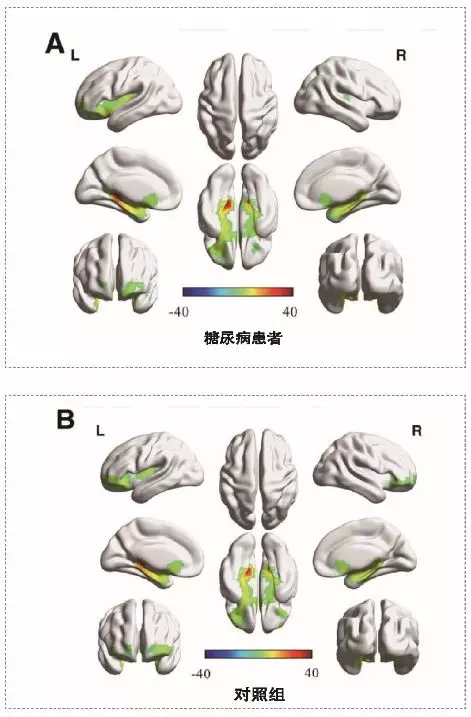
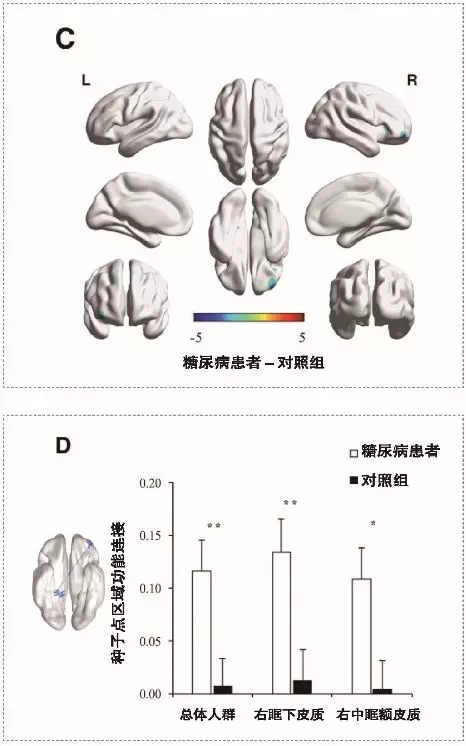
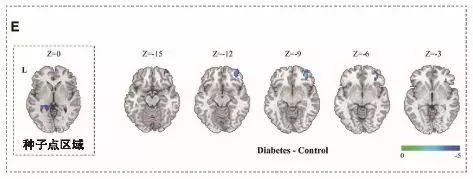
近期,南京大学医学院附属鼓楼医院内分泌科朱大龙教授、毕艳教授研究首次发现,在2型糖尿病患者表现认知衰退症状前,嗅觉相关脑区已发生激活改变。受损的嗅觉脑区功能连接与神经心理测试、嗅觉行为学测试得分呈正相关,为糖尿病相关认知障碍的早期预测和评估提供了重要的新线索。(Diabetes 2018;67:1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#DIA#
35
#Diabetes#
40
#BET#
25
学习了受益匪浅
55
学习了
55
学习了.长知识
62