JCI:北大人民医院申占龙团队揭示亚洲人特异性的IgG1记忆性B细胞抗原受体变异体对结直肠癌微环境中的作用机制
2022-04-08 北大人民医院 北大人民医院
2022年3月15日,北京大学人民医院胃肠外科申占龙课题组与清华大学生命科学学院免疫学研究所刘万里课题组合作攻关,在IgG1记忆性B淋巴细胞调控结直肠肿瘤免疫微环境研究领域取得重要进展,在国际著名生物
2022年3月15日,北京大学人民医院胃肠外科申占龙课题组与清华大学生命科学学院免疫学研究所刘万里课题组合作攻关,在IgG1记忆性B淋巴细胞调控结直肠肿瘤免疫微环境研究领域取得重要进展,在国际著名生物医学杂志Journal of Clinical Investigation发表研究论文“An Asian-Specific Variant in Human IgG1 Represses Colorectal Tumorigenesis by Shaping the Tumor Microenvironment”,揭示了亚洲人特异性的IgG1记忆性B细胞抗原受体膜联免疫球蛋白IgG1重链基因的单核苷酸多态性变异体(简称为hIgG1-G396R)抵御结直肠癌发生发展,并分析了IgG1记忆性B细胞在重塑肿瘤抗癌微环境中的作用机制和潜在应用。
T细胞在肿瘤免疫逃逸和作为药物治疗靶点的重要性已经获得公认,但是对B细胞的研究相对较少。最近研究发现,B细胞在几种癌症类型(包括乳腺瘤、黑素瘤、结直肠癌、卵巢癌等)的发生发展中发挥重要作用。申占龙课题组前期在结直肠免疫细胞图谱的刻画工作中发现,B细胞与T细胞、DC细胞具有互作关系(Cell,2020),但是B细胞在复杂的肿瘤微环境中通过何种机理发挥作用尚未完全清楚。合作者刘万里课题组前期和北京大学人民医院风湿免疫科栗占国课题组研究发现亚洲人特异性的hIgG1-G396R变异体增强了B细胞活性,增加了系统性红斑狼疮的易感性 (Science, 2018)。hIgG1-G396R变异体是否在肿瘤发生发展中发挥保护性作用尚属未知。申占龙课题组联手刘万里课题组围绕hIgG1-G396R在结直肠癌中的作用和机制展开联合研究。
研究者们对一千余例结直肠癌患者队列进行流调分析,发现hIgG1-G396R纯合基因型的肿瘤患者可以明显改善总体预后生存和无进展预后生存,多因素COX风险分析揭示hIgG1-G396R纯合基因型对于结直肠癌患者是独立的保护性预后生存因素。进一步研究发现,与携带野生型、hIgG1-G396R杂合子患者相比,携带hIgG1-G396R纯合子结直肠癌患者的肿瘤组织有更多的浆细胞、CD8+T细胞和DC细胞浸润以及TLS(三级淋巴结结构)形成。hIgG1-G396R同源体小鼠的肿瘤微环境得到类似结果,并检测到更高水平的IgG抗体、IFN-γ和颗粒酶B表达。单细胞转录组数据分析发现在携带hIgG1-G396R结直肠癌患者的肿瘤组织中,浆细胞、TH细胞和记忆性T细胞增加,而耗竭性T细胞减少。这提示我们,记忆性B细胞抗原受体hIgG1-G396R变异体不仅影响了肿瘤组织中浆细胞的分化和肿瘤特异性抗体的产生,还可以重塑肿瘤免疫微环境,动员T细胞和DC细胞发挥更强的抗肿瘤能力。研究者们还发现,过继输注hIgG1-G396R同源体小鼠体内的高反应性B细胞可减缓结肠肿瘤的生长速度,具有抗肿瘤作用。
上述研究说明hIgG1-G396R变异体可能是结直肠癌患者的重要保护性预后因素,揭示hIgG1-G396R在结直肠癌领域具有作为患者预后指标的应用潜力,为患者的生存预测、用药指导等提供参考价值,也提示IgG1+ B细胞过继转移可能是癌症免疫疗法的有力策略之一,并激励更多的研究者们探索将B细胞应用于免疫治疗的可能性。这一系列的研究结果加深了人们对记忆性B细胞在结直肠癌中的功能和保护性免疫学机制的认识,为临床不同基因型结直肠癌患者的预后水平和临床病理特征进行合理的预测,也为记忆性B细胞进行过继转移治疗癌症提供了创新性的研究模式。
刘万里课题组已毕业的杨冰博士、申占龙课题组已毕业的张振博士、刘万里课题组队已毕业的陈相军博士为本文的并列第一作者。刘万里和申占龙为论文共同通讯作者。该研究得到北京大学张泽民教授、周晓华教授,中山大学邝栋明教授,深圳湾实验室张雷研究员,北京大学人民医院栗占国教授、王杉教授、叶颖江教授,复旦大学吴凡教授、黄竞荷教授、陆路研究员,中国科学院生物物理研究所李岩教授,清华大学祁海教授等多位老师的大力支持。
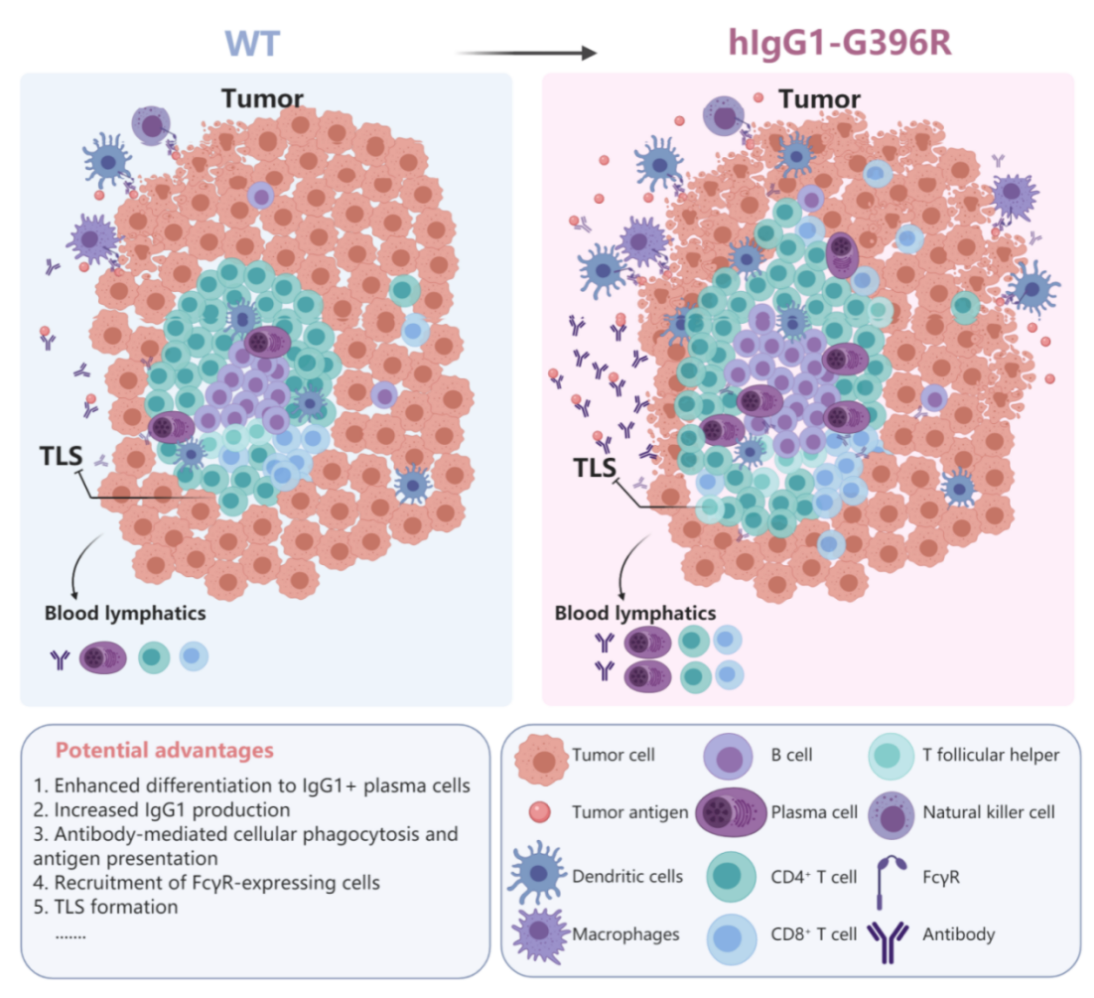
IgG1记忆性B细胞抗原受体膜联重链hIgG1-G396R变异体重塑结直肠癌肿瘤微环境,并增强抗肿瘤免疫力的示意图。左侧为对照组,右侧为hIgG1-G396R纯合基因型肿瘤患者增强的抗肿瘤免疫微环境:包括增强的TLS结构和功能,增加的IgG1+浆细胞分化和浸润,上调的IgG1抗体浸润,进而通过抗体恒定区调理效应发挥功能(ADCP、ADC等)
专家介绍
申占龙,北京大学人民医院胃肠外科主任医师,教授,博士生导师,外科肿瘤研究室副主任。课题组围绕胃肠肿瘤免疫微环境开展了系列创新研究,包括:揭示肿瘤相关巨噬细胞(TAM)促侵袭转移特性和系列分子机制,通过联合研究首次在单细胞水平揭示结直肠癌T细胞动态变化,从单细胞精度揭示与PD-1/PD-L1抑制剂治疗获益相关T细胞新类群,成功构建可以有效筛选PD-L1抑制剂治疗获益患者的免疫微环境评分,从单细胞精度揭示以TAM细胞和树突状细胞(DC)为靶点的免疫治疗新机理,发现PD-1抑制剂与化疗药5-Fu联用治疗效果更好的泛素化调控新机制,研究成果以通讯作者(含共同)发表于Nature、Cell、J Clin Invest、PNAS、EMBO Reports、Npj Genomic medicine等,先后荣获:细胞出版社2020中国年度论文、 2020年度“敬佑生命﹒荣耀医者”青年创新奖、北京市科学技术奖-自然科学奖一等奖、韩国国际胃癌学术周最佳报告奖、首届北京大学杰出青年医师奖等。兼任:中国医师协会外科医师分会MDT学组副秘书长/青年委员会主任委员,中华医学会外科学分会实验外科学组委员,美国外科学院Fellow(FACS)等。
原始出处:
Yang B, Zhang Z, Chen X, Wang XY, Qin S, Du L, Yang C, Zhu L, Sun W, Zhu Y, Zheng Q, Zhao S, Wang Q, Zhao L, Lin Y, Huang J, Wu F, Lu L, Wang F, Zheng W, Zhou XH, Zhao X, Wang Z, Xiao-Lin S, Ye Y, Wang S, Li Z, Qi H, Zhang Z, Kuang DM, Zhang L, Shen Z, Liu W.An Asia-specific variant of human IgG1 represses colorectal tumorigenesis by shaping the tumor microenvironment.J Clin Invest. 2022 Mar 15;132(6):e153454. doi: 10.1172/JCI153454
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCI#
38
#北大人民医院#
56
#人民医院#
51
#特异性#
30
#变异体#
44
#记忆性#
29
#B细胞#
32
#变异#
25
#结直肠#
33
#IgG#
35