Lancet Oncol:双雄相争 谁才是转移性结直肠癌的更佳二线治疗?
2018-06-08 徐钰琦 环球医学
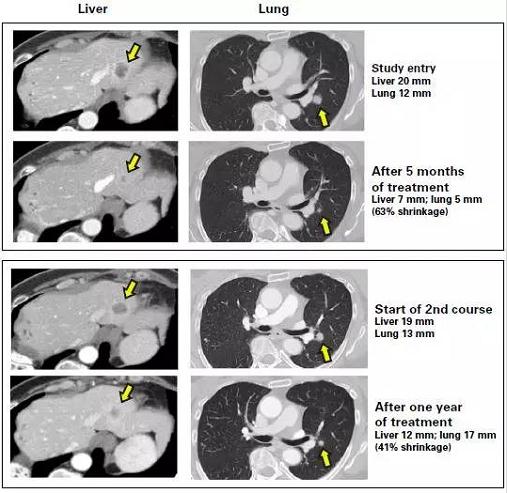
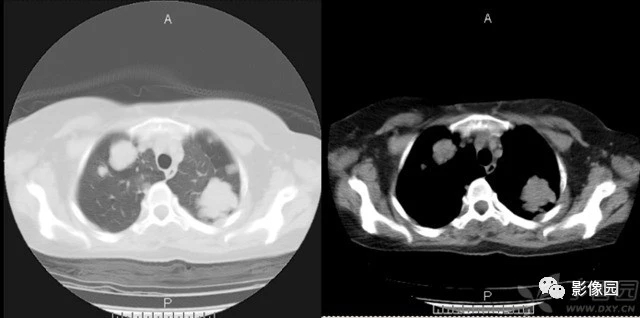
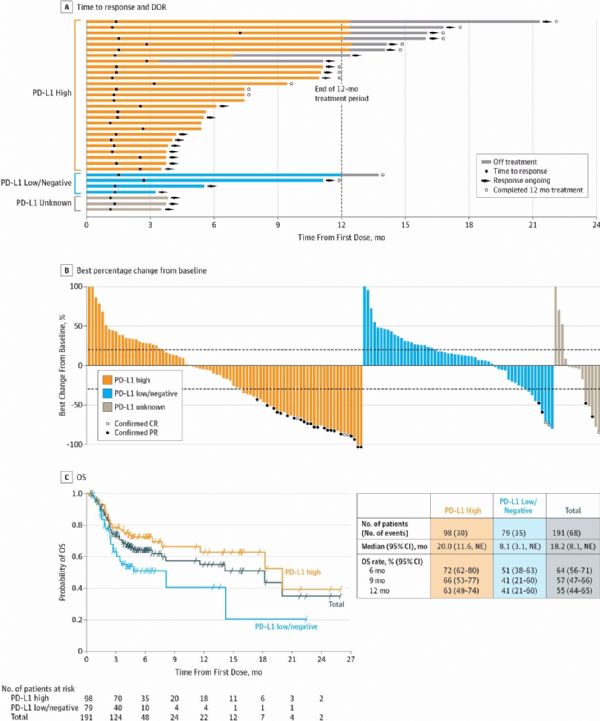
2018年5月,发表于《Lancet Oncol》上的一项多中心、开放性、随机、非劣效性3期试验,考察了改良XELIRI(mXELIRI:卡培他滨+伊立替康)vs FOLFIRI(亚叶酸钙,氟尿嘧啶和伊立替康),两者联用/不联用贝伐珠单抗,作为转移性结直肠癌二线治疗的有效性和安全性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
29
#Oncol#
20
了解一下谢谢
45
可以尝试
58
学习了
48
#转移性#
20
#结直肠#
20
#二线治疗#
24
希望以后更多的进展可以及时推送
60
了解一下.谢谢分享!
55