Eur Heart J:含钠对乙酰氨基酚与心血管结局的关系
2022-02-26 MedSci原创 MedSci原创
在患有或不患有高血压的参与者中,服用含钠对乙酰氨基酚与心血管疾病风险和全因死亡率增加相关。该研究的结果表明个体应避免服用含钠对乙酰氨基酚来避免不必要的过量钠摄入。
先前的研究发现,较高的钠摄入量与高血压患者心血管疾病(CVD)风险和全因死亡率增加相关;关于摄入量对无高血压个体影响的研究结果目前尚未明确。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员的目的是根据高血压病史,比较含钠的对乙酰氨基酚初始服用者与不含钠制剂的同一药物服用者的心血管疾病和全因死亡率风险。
研究人员使用健康改善网络,在患有和不患有高血压的个体中进行了两项队列研究。研究人员使用具有逆概率加权的边际结构模型评估了含钠对乙酰氨基酚与1年随访期间每个结局风险之间的关系,以调整随时间变化的混杂因素。该研究的结局是心血管疾病事件(心肌梗塞、卒中和心力衰竭)和全因死亡率。
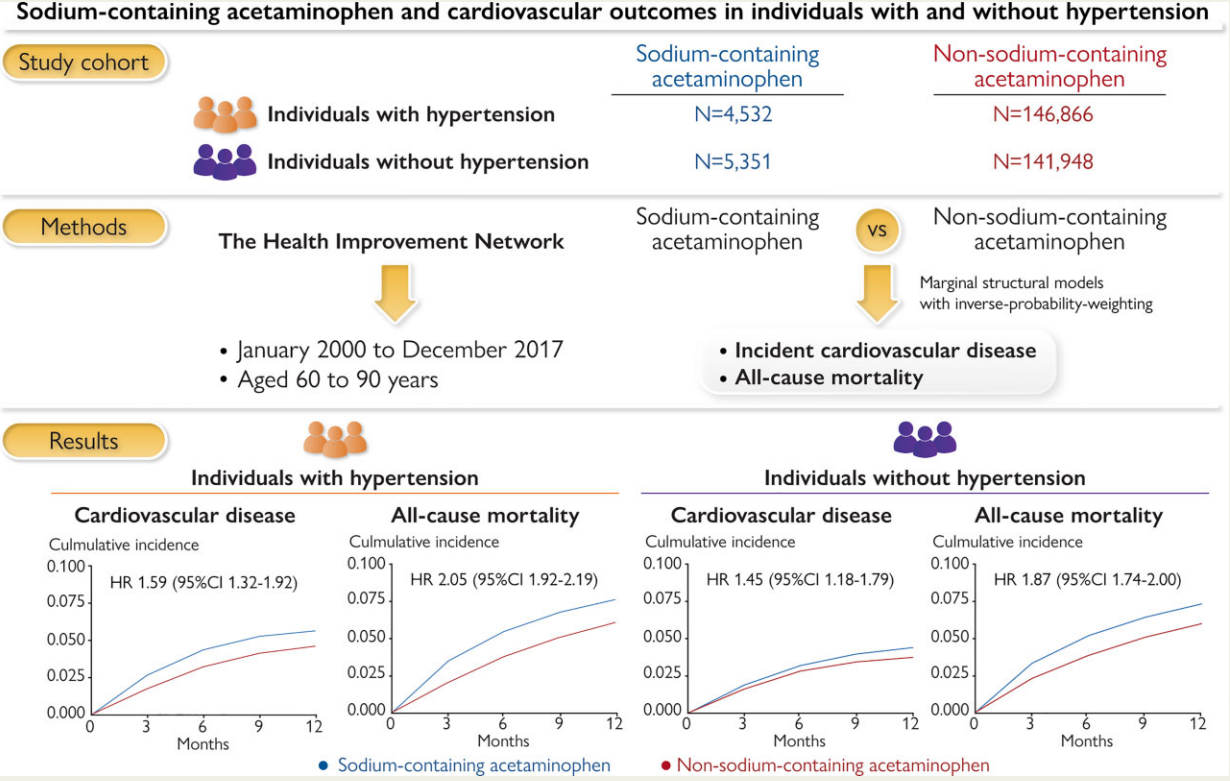
在高血压患者(平均年龄为73.4岁)中,4532名含钠对乙酰氨基酚服用者发生了122例CVD(1年风险为5.6%),146866名非钠对乙酰氨基酚服用者中有3051例(1年风险为4.6%)。平均加权风险比(HR)为1.59[95%置信区间(CI)为1.32–1.92]。在没有高血压的参与者(平均年龄为71.0岁)中,5351名含钠对乙酰氨基酚服用者发生了105例CVD(1年风险为4.4%),141948名非含钠对乙酰氨基酚服用者中有2079例(1年风险为3.7%),平均加权HR为1.45(95%CI为1.18–1.79)。特定CVD结局和全因死亡率的结果相似。
由此可见,在患有或不患有高血压的参与者中,服用含钠对乙酰氨基酚与心血管疾病风险和全因死亡率增加相关。该研究的结果表明个体应避免服用含钠对乙酰氨基酚来避免不必要的过量钠摄入。
原始出处:
Chao Zeng,et al.Sodium-containing acetaminophen and cardiovascular outcomes in individuals with and without hypertension.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac059/6535634
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乙酰氨基酚#
47
#心血管结局#
70
#对乙酰氨基酚#
48
#ART#
40
#HEART#
42
学习学习
54
受教了
63