Lancet oncol:滤泡性淋巴瘤患者经一线免疫化疗后,以PET评估缓解情况的效果优于增强CT
2018-10-09 MedSci MedSci原创
正在进行的GALLIUM试验的初步结果表明滤泡性淋巴瘤患者采用奥比托珠单抗进行一线免疫化疗后的无进展存活期要比用利妥昔单抗化疗的长。现研究人员对该试验进行二次分析评估GALLIUM试验中一线免疫化疗后PET-CT反应的预后意义。GALLIUM是一个开放标签的平行随机的3期试验,招募年满18岁的既往未治疗过的CD22阳性的滤泡性淋巴瘤患者(1-3a级、III/IV期或II期+肿瘤最大直径≥7cm)。
GALLIUM是一个开放标签的平行随机的3期试验,招募年满18岁的既往未治疗过的CD22阳性的滤泡性淋巴瘤患者(1-3a级、III/IV期或II期+肿瘤最大直径≥7cm)。将患者随机按1:1随机分至奥比托珠单抗组(第1疗程的第1、8和15天,和随后每疗程的第1天,1000mg 静滴)或利妥昔单抗组(每疗程第1天 375mg/m2 静滴),主要结点是已报道过的无进展存活期。二次分析主要是在诱导治疗结束后,以PET和CT为基础的缓解评估,并解释其与无进展存活期和总体存活预后之间的关系。
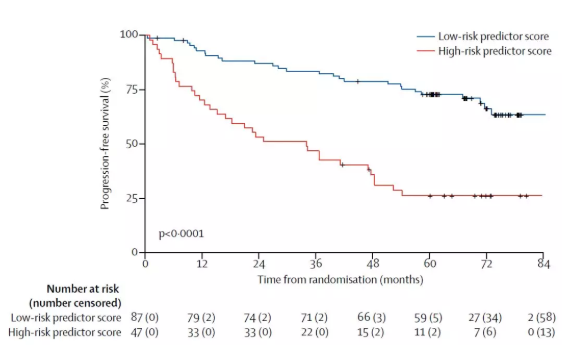
2011年7月6日-2014年2月4日共招募了1202位患者,其中595位被纳入PET人群;533(IHP 2007;前瞻性分析)和508位(Lugano 2014,回顾性分析)进行无进展存活期分析。诱导结束时,595位患者中有390位(65.5%[95% CI 61.6-69.4])获得PET完全缓解(根据IHP 2007标准),450位(75.6%[95% CI 72.0-79.0])获得PET完全代谢缓解(根据Lugano2014标准)。观察中位时间43.3个月(IQR 36.2-51.8),根据IHP 2007标准,PET完全应答者和未完全应答者诱导结束后2.5年无进展存活率分别达到87.8%(95% CI 83.9-90.8)和72.0%(95% CI 63.1-79.0;HR 0.4,95% CI 0.3-0.6,p<0.0001)。根据Lugano 2014标准,完全代谢应答者和未完全应答者的2.5年无进展存活率分别是87.4%(95% CI 83.7-90.2)和54.9%(40.5-67.3;HR 0.2,95% CI 0.1-0.3,p<0.0001)。
本研究表明在滤泡性淋巴瘤患者经过一线免疫化疗后,用PET来评估缓解情况比增强CT的效果好。根据Lugano 2014缓解标准PET评估,PET评估为研究缓解适应性的治疗措施提供平台。
原始出处:
Judith Trotman,et al. Prognostic value of end-of-induction PET response after first-line immunochemotherapy for follicular lymphoma (GALLIUM): secondary analysis of a randomised, phase 3 trial. The Lancet Oncology. October 08,2018.https://doi.org/10.1016/S1470-2045(18)30618-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
31
#Oncol#
24
#Lancet#
31
#增强CT#
32
#滤泡性淋巴瘤#
35
#PET#
27
很牛的数据
0
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
40
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
73
学习
65