J Cardiol:ALPACS研究结果出人意料 非ST抬高心梗介入术前负荷他汀无获益
2015-05-08 中国循环杂志 中国循环杂志
近期,中山医院葛均波教授牵头的ALPACS研究显示,对于非ST段抬高急性心肌梗死患者,PCI前负荷应用80 mg阿托伐他汀没有减少术后30天不良事件,也没有降低围手术期心肌梗死发生率。 作者表示,该研究结果与ARMYDA-ACS的设计相似,ARMYDA-ACS研究公布之后,也有Meta分析证明PCI前启动他汀有益处,其中也包括了亚洲患者,但“我们研究的结果出乎意料。”[pdf free] 该研
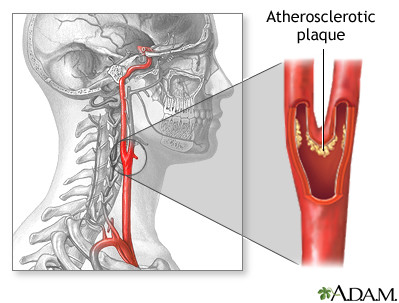
近期,中山医院葛均波教授牵头的ALPACS研究显示,对于非ST段抬高急性心肌梗死患者,PCI前负荷应用80 mg阿托伐他汀没有减少术后30天不良事件,也没有降低围手术期心肌梗死发生率。
作者表示,该研究结果与ARMYDA-ACS的设计相似,ARMYDA-ACS研究公布之后,也有Meta分析证明PCI前启动他汀有益处,其中也包括了亚洲患者,但“我们研究的结果出乎意料。”[pdf free]
该研究表明,对于亚洲ACS患者,在PCI前12小时和2小时再给予阿托伐他汀负荷剂量80 mg和20 mg,随访30天时发现,负荷他汀无明显获益(图1)。他汀负荷量组主要不良心脏事件发生率为15%,而在常规治疗组为16%。
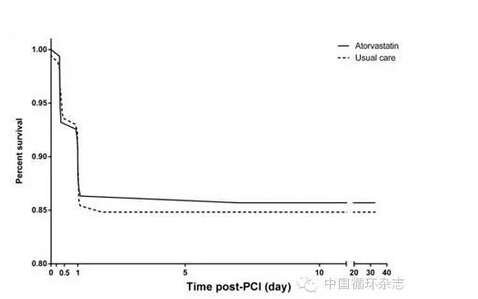
事后分析显示,在PCI后8小时,负荷组CK-MB升高≥3倍的比例为3.82%,24小时的比例为7.64%,而常规组两个时间段的比例分别为7.22%和9.47%。两组在心肌肌钙蛋白I、肌红蛋白以及C反应蛋白等相比也无差异。

作者认为,该研究没有得到ARMYDA-ACS研究的结论,可能与诊断标准和操作水平等有一定关系。ARMYDA-ACS研究中,34%阿托伐他汀组是多支血管病变,但仅有20%的患者进行了多支血管介入治疗。还有,ARMYDA-ACS研究仅64%的人使用了药物洗脱支架,而中韩两国使用药物洗脱支架的比例较高。
另外,ALPACS研究确实观察到对照组CK-MB升高的比例较高,但该研究没有围手术期症状和影像学变化,而是采用肌钙蛋白诊断围手术期心梗,但已有研究表明,用肌钙蛋白诊断围手术期太敏感。
ALPACS研究是一前瞻性、多中心研究,共纳入499位接受他汀初始治疗的非ST段抬高ACS患者,均计划接受PCI。这些患者均服用阿托伐他汀40 mg/d。其中,247位患者则在此基础上,PCI前12小时再给予80 mg阿托伐他汀,2小时前给予40 mg。最终335位患者进行了PCI,包括术前给予他汀负荷量的163位患者。主要心脏不良事件包括死亡、心肌梗死以及靶血管重建。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cardiol#
33
#ALP#
22
#前负荷#
37
#研究结果#
19
还没有定论
56
#ACS#
25
#LPA#
19
有争议
103
看看
88
了解
86