JCEM:在患有21-羟化酶缺乏症的先天性肾上腺增生的成人中,Crinecerfont可以降低该疾病升高的激素标志物
2022-03-26 从医路漫漫 网络
先天性肾上腺增生症(CAH)是一组罕见的常染色体隐性遗传病,导致肾上腺类固醇合成紊乱,包括皮质醇合成受损。
背景:先天性肾上腺增生症(CAH)是一组罕见的常染色体隐性遗传病,导致肾上腺类固醇合成紊乱,包括皮质醇合成受损。由于21-羟基酶缺乏(210HD)的CAH患者会产生过量的肾上腺雄激素,这一人群约占所有CAH病例的95%。皮质醇缺乏消除了对下丘脑和脑垂体的正常负反馈抑制,导致下丘脑分泌的促肾上腺皮质激素释放因子和脑垂体分泌的促肾上腺皮质激素(ACTH)增加。慢性ACTH驱动导致肾上腺雄激素过量产生由21-OHD引起的“经典”形式的CAH,与更严重的酶缺乏症有关,发生率约为1:15000。胎儿期雄激素过多导致46,XX新生儿男性化;21-OHD是女婴非典型生殖器的主要原因。儿童期和青春期持续的雄激素过多会导致性早熟、男性化,并随着骨龄的延长而加速身体生长,最终导致低于预期的成人身高。成年期间,多毛症和月经不调在女性中很常见,患有21OHD的男性和女性会遭受生育能力下降和精神障碍的困扰。此外,所有患有21OHD的患者都有肾上腺危象的风险,如果不治疗,可能导致死亡。
糖皮质激素(GC)疗法是目前的治疗标准,用于替代内源性皮质醇缺乏症。然而,通常需要超生理GC剂量和非生理时间(如晚上给药)来减少ACTH分泌增加和雄激素分泌过多。这种超生理GC剂量的慢性暴露会导致严重的并发症,包括儿童生长抑制、骨密度降低和骨折风险增加,以及代谢紊乱,如肥胖、胰岛素抵抗和高血压,这些都会增加心血管风险。因此,治疗21-OHD的挑战是平衡雄激素的充分控制与过度和长期GC暴露的风险;GCs治疗不足和过度都会引起副作用和并发症。
促肾上腺皮质激素释放因子1型受体(CRF1R)的拮抗剂可能为治疗这种疾病提供一种新的方法。CRF1R拮抗作用可以减少ACTH分泌,这在21OHD中可以减少雄激素的下游产生并减少雄激素过多症的症状,同时也潜在地允许GCs以更多的生理剂量给药。因此,这种方法有助于减轻长期超生理GC治疗的负面影响。在一项CRF1R拮抗剂(NBI-77860)的探索性研究中证明了CRF1R拮抗剂的潜在功效,该研究对8名患有21OHD的女性患者进行了研究,发现单剂量给药后ACTH和17-羟孕酮(17OHP)有意义的减少。
一种口服的非甾体类CRF1R拮抗剂,目前正在研究用于治疗经典的21-OHD。本2期研究(NCT03525886)旨在评估本品的安全性、耐受性以及对患有典型21OHD的成人促肾上腺皮质激素、肾上腺雄激素和雄激素前体的影响。
目的:本研究旨在评价CRF1R选择性拮抗剂CRI-74788治疗21OHD的安全性、耐受性和有效性。
方法:采用序贯队列设计(NCT03525886),在美国的6个中心进行了这项开放标签的第2阶段研究。参与者包括男性和女性,年龄在18岁到50岁之间,患有21OHD。干预措施包括4种CRINECERFONT方案,每种方案连续14天口服:每天睡前服用一次50或100毫克(队列1和2);每天晚上服用100毫克(队列3);每天两次100毫克(队列4)。参与者可以注册一个以上的队列。主要结果包括从基线到第14天促肾上腺皮质激素(ACTH)、17-羟孕酮(17OHP)、雄烯二酮和睾酮的变化。
结果:18例受试者中,女性11例,男性7例,队列1 8例,队列2 7例,队列3 8例,队列4 8例。平均年龄为31岁;94%是白人。ACTH(-66%)、17OHP(-64%)和雄烯二酮(-64%)每天两次服用100 mg,平均下降60%以上。在女性参与者中,73%(8/11)的人睾酮水平下降了50%或更多;男性参与者的雄烯二酮/睾酮比率下降了中位数26%至65%。

图1 学习设计。蓝色三角形表示样本收集。在所有队列中,24小时基线期(第7天至第6天)的取样与内分泌治疗期间的取样时间表相匹配。对于基线和第1天访视,参与者在10:00(晨窗结束)采集样本后接受其处方糖皮质激素剂量;对于第14天的访视,在14:00采集样本后给予糖皮质激素。GC糖皮质激素。
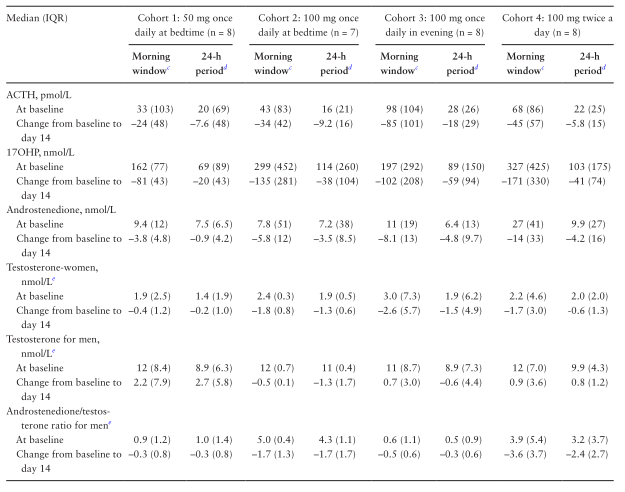
表1 雌激素对肾上腺雄激素和前体的影响
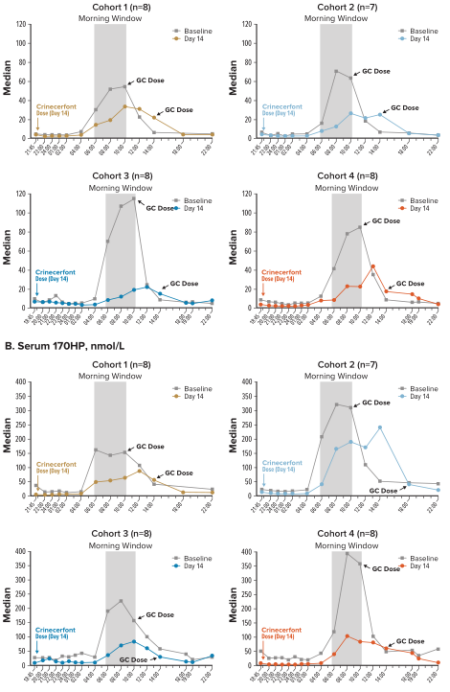
图2 对于第1组和第2组,在第14天的22:00给药;给药前取样时间为21:45。对于第3组和第4组,在第14天的19:00给药;给药前取样时间是18:45。17OHP,17-羟孕酮;促肾上腺皮质激素;GC糖皮质激素。

图3。从基线到第14天基于早晨窗值的百分比减少中值。基于早上时段时间点(06:00、08:00、10:00)每个参与者的值。中值百分比减少的四分位数范围(Q3-Q1的绝对值)显示在括号中。17OHP,17-羟孕酮;促肾上腺皮质激素。
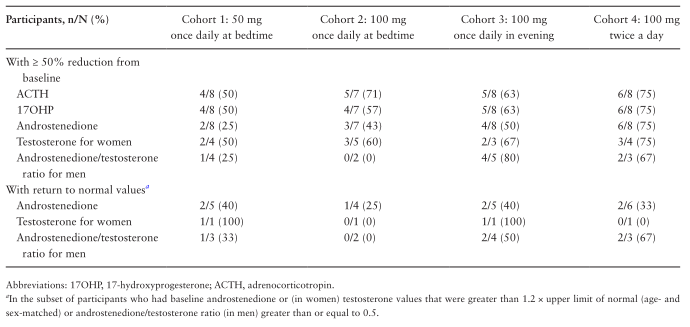
表2 从基线到第14天,晨窗激素值减少50%或更多的参与者比例,以及达到正常值的比例
结论:在成人21OHD患者中,Crinecerfont治疗14天可降低ACTH,并对升高的17OHP、雄烯二酮、睾酮(女性)或雄烯二酮/睾酮比值(男性)有临床意义的降低。需要更长期的研究来评估Crinecerfont对21OHD患者激素合成紊乱和糖皮质激素暴露的临床终点的影响。
原文出处:Auchus RJ, Sarafoglou K, Fechner PY, et al.Crinecerfont Lowers Elevated Hormone Markers in Adults With 21-Hydroxylase Deficiency Congenital Adrenal Hyperplasia.J Clin Endocrinol Metab 2022 02 17;107(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#标志物#
32
#先天性肾上腺增生#
37
#肾上腺#
36
#JCE#
47
#JCEM#
38
#NEC#
39
#先天性#
35