JAHA:花粉浓度的时间变化预测急性冠状动脉综合征的短期临床结局
2022-03-17 MedSci原创 MedSci原创
花粉浓度增加与不同的ACS亚型无关,但与经皮冠状动脉介入治疗后的住院死亡率显著相关,强调了花粉暴露与临床结局之间的潜在生物学联系。
一些观察性研究已将特定疾病状态的发生发展与环境因素变化联系起来,例如哮喘的恶化。吸入空气的可变性和质量就是这样的环境因素之一。由于空气传播的花粉含量的变化或人类活动导致污染物和空气传播的颗粒物的变化,吸入空气成分的变化可能会自然发生。花粉浓度的变化可能会通过引发各种过敏过程来影响人类健康。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员试图评估花粉浓度的变化是否与不同的急性冠状动脉综合征(ACS)亚型表现和短期临床结局之间的相关性。
研究人员分析了2014年1月至2017年12月期间接受经皮冠状动脉介入治疗的患者,并比较暴露于不同草木和总花粉浓度的患者基线特征。该研究的主要结局是发生ACS亚型和30天主要不良心脑血管事件(死亡率、心肌梗死、支架血栓形成、靶血管血运重建或卒中)。
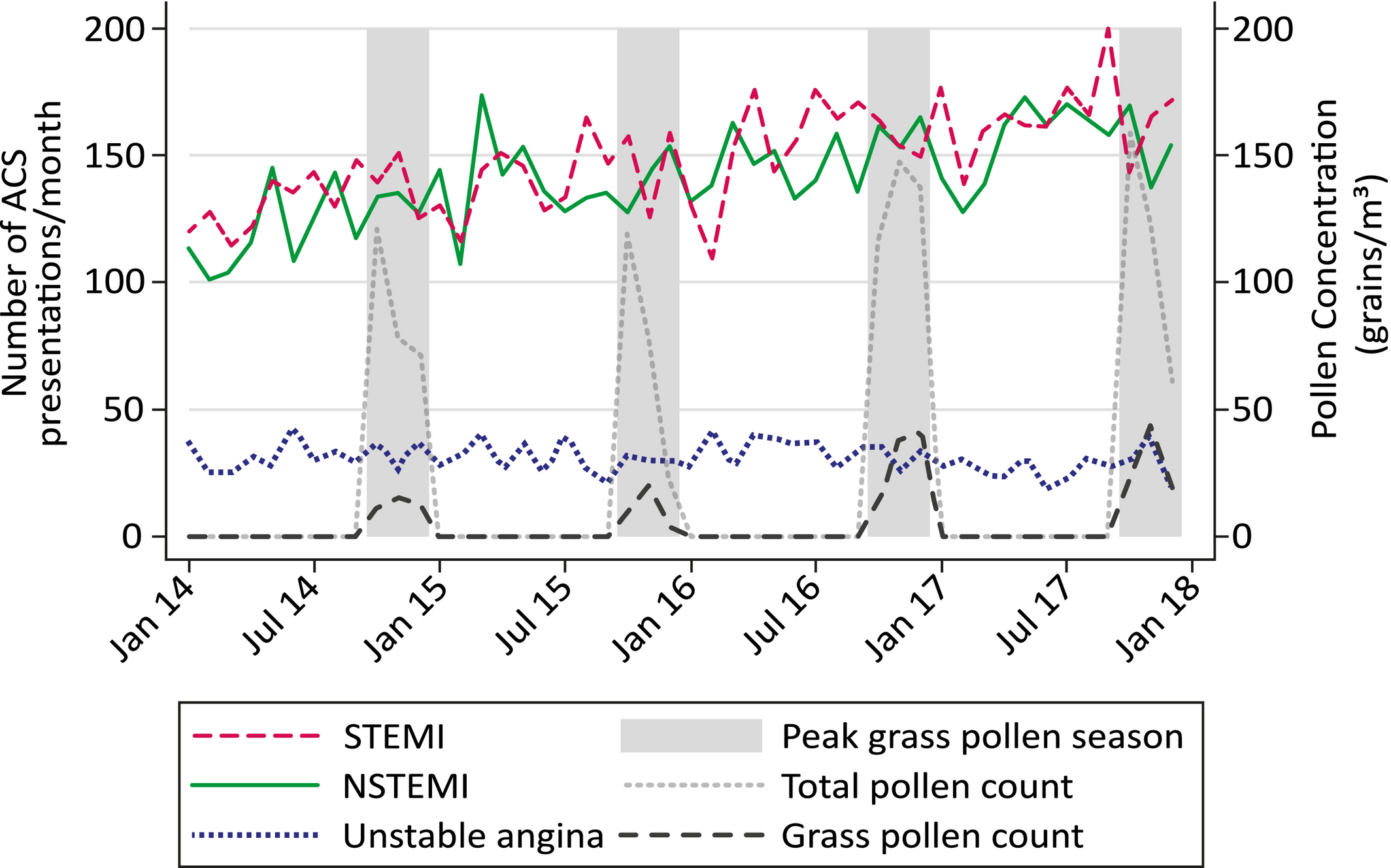
在15379例患者中,7122例(46.3%)患者出现ST段抬高型心肌梗死,6781例(44.1%)患者出现非ST段抬高型心肌梗死,1476例(9.6%)患者出现不稳定型心绞痛。平均年龄为62.5岁,男性占患者的76%。研究人员没有观察到每日或季节性草木和总花粉浓度与ACS亚型出现频率之间的关联。然而,前几天的草木和总花粉浓度(草花粉的2天平均值和总花粉的7天平均值)与住院死亡率(比值比[OR]为2.17[95%CI为1.12-4.21];P=0.021和OR为2.78[95%CI为1.00-7.74];P=0.05)和30天主要不良心脑血管事件(OR为1.50[95%CI为0.97-2.32];P=0.066)相关。
由此可见,花粉浓度增加与不同的ACS亚型无关,但与经皮冠状动脉介入治疗后的住院死亡率显著相关,强调了花粉暴露与临床结局之间的潜在生物学联系。
原始出处:
Omar Al‐Mukhtar.et al.Temporal Changes in Pollen Concentration Predict Short‐Term Clinical Outcomes in Acute Coronary Syndrome.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.023036
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠状动脉综合征#
38
#临床结局#
44
#AHA#
30
#花粉#
41
#综合征#
26
#浓度#
45
学习
43
实用
43