ASCO GU 2021: HIF-2α抑制剂Belzutifan在晚期肾透明细胞癌中初显疗效
2021-02-16 MedSci原创 MedSci原创
Belzutifan(MK-6482)是一种小分子HIF-2α抑制剂,临床前研究已证实可诱导肾细胞癌模型的肿瘤消退,此前也报道了首个人类实体瘤的Ⅰ期研究。2021年ASCO GU大会口头报
Belzutifan(MK-6482)是一种小分子HIF-2α抑制剂,临床前研究已证实可诱导肾细胞癌模型的肿瘤消退,此前也报道了首个人类实体瘤的Ⅰ期研究。2021年ASCO GU大会口头报告中,一项MK-6482单药治疗的Ⅰ/Ⅱ期研究以及一项MK-6482联合卡博替尼的Ⅱ期研究再传捷报,HIF-2α抑制剂在晚期肾癌治疗中显露出不俗的潜力!
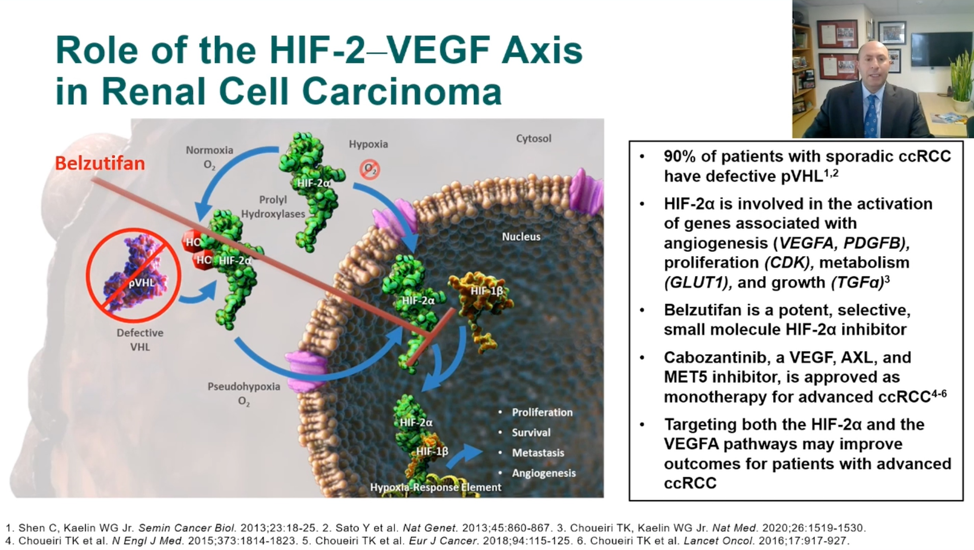
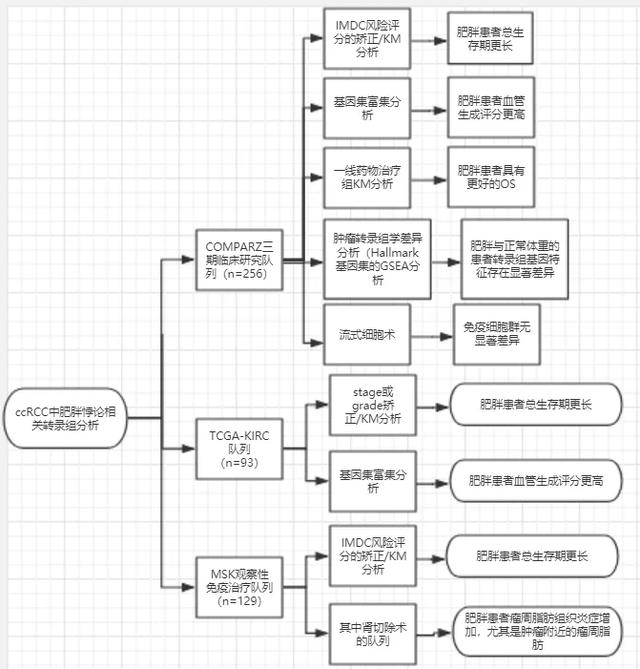
Toni Choueiri博士介绍了belzutifan(MK-6482)与美国联邦药物管理局(FDA)批准的多种TKI,卡巴替尼结合的2期研究的初步结果。 正如在今年的美国临床肿瘤学会泌尿生殖道癌症研讨会(ASCO GU)上的其他演讲所介绍的那样,超过90%的透明细胞肾细胞癌(ccRCC)患者具有偶发的基因组改变,从而导致缺陷的VHL蛋白和假性低氧状态。 后一点是用belzutifan靶向HIF2alpha的基本原理。
在美国,透明细胞癌(ccRCC)约占肾癌病例的70%。一些一线治疗已被批准用于ccRCC,但很少有患者可达到完全缓解,大多数患者在5~11个月内发生进展。RCC的一个关键致癌因子是转录因子缺氧诱导因子2α(HIF-2α)。MK-6482则是一种小分子HIF-2α抑制剂,可阻断HIF-2α与HIF-1β的异源二聚,诱导小鼠移植肾细胞癌模型的肿瘤消退。
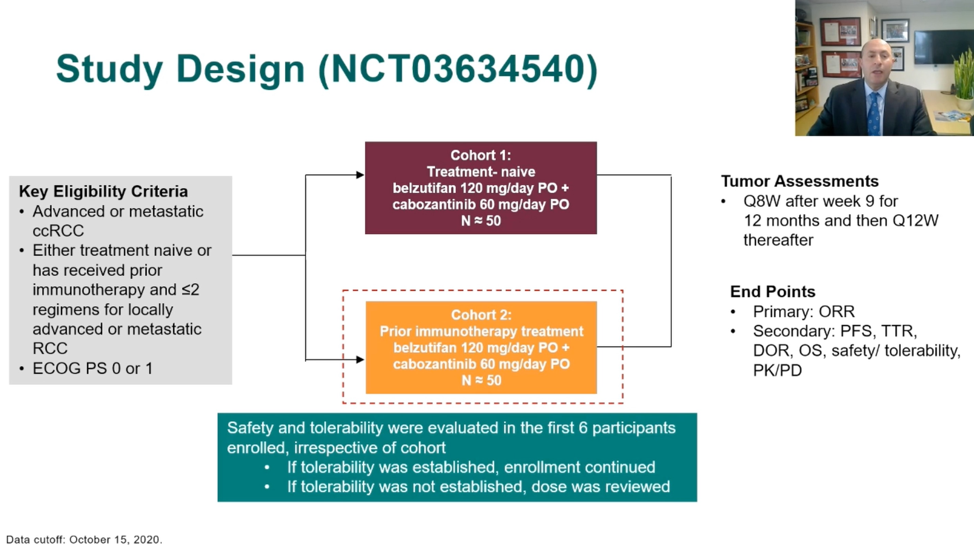
HIF-2α抑制剂Belzutifan(MK-6482)在转移性ccRCC患者的Ⅰ期研究中已被证明具有良好的抗肿瘤活性和安全性。这项研究(NCT03634540)进一步探讨Belzutifan联合卡博替尼治疗晚期ccRCC患者的疗效,这些患者为初次治疗(队列1)或既往接受过免疫治疗和TKIs治疗(队列2)。
该研究由两组晚期透明细胞RCC患者组成。 在队列1中,患者未接受过治疗; 在队列2中,患者先前曾接受过免疫治疗和/或TKI。 演讲的重点是队列2的初步结果。
在队列2中,所有受试者均为转移性肾透明细胞癌(ccRCC),且既往接受过的系统治疗方案不超过2种。在研究之初,队列1或队列2中有6例患者每天口服一次Belzutifan(120 mg)联合卡博替尼(60 mg),持续21天,由此确定Ⅱ期推荐剂量(RPTD)。
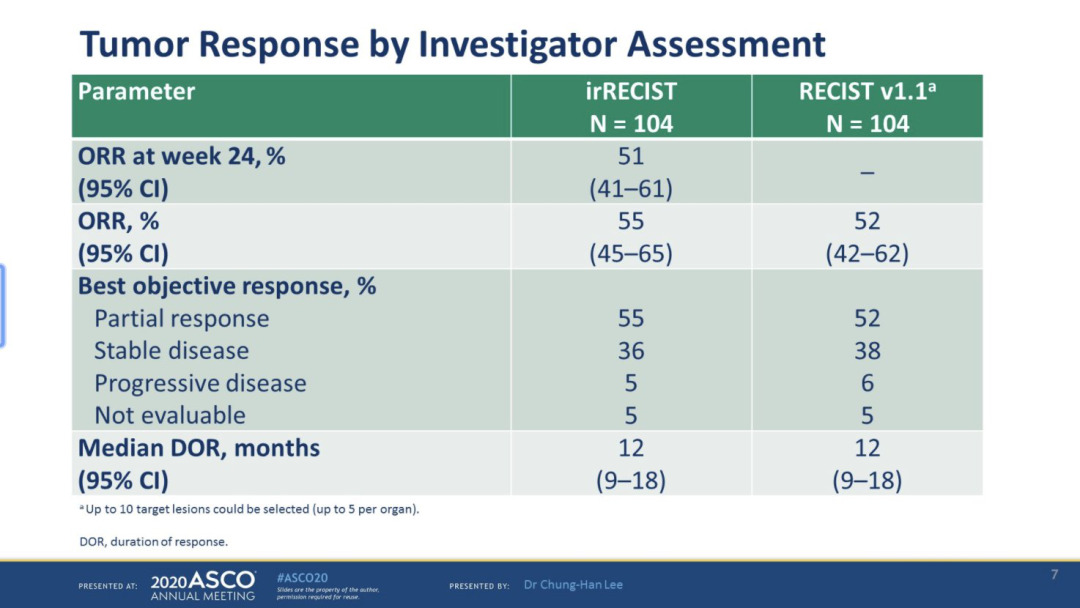
此次的初步分析提供了队列2的数据,对接受≥1剂量治疗并随访≥6个月的患者进行疗效评估。主要终点为研究者根据RECIST v1.1评估的观缓解率(ORR)。次要终点包括无进展生存期(PFS)、总生存期(OS)和缓解持续时间(DOR)。对所有队列参与者进行安全性评估。
53例患者被纳入安全性分析人群。中位年龄64岁,73.6%为男性,54.7%为ECOG 状态1分。28例(52.8%)接受过一线治疗,24例(45.2%)接受过二线治疗。随访≥6个月的患者(n=41)从登记到数据截止的中位随访时间为11.3个月(范围:5.6-24.0)。
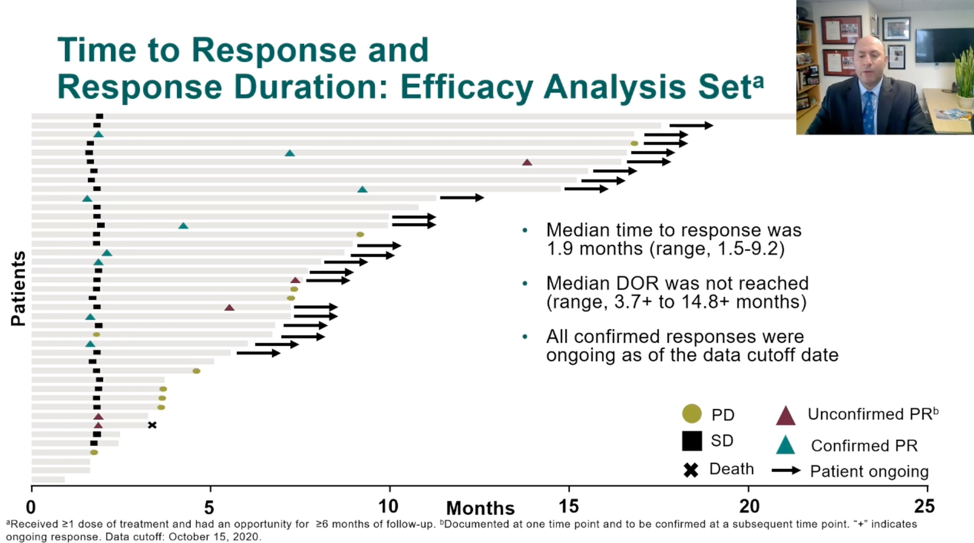
ORR为22.0%(9例达到PR),90.2%有肿瘤缩小。疾病控制率(CR+PR+SD)为92.7%。中位DOR未到达(范围:3.7+ ~ 14.8+个月)(cutoff时间为2020年10月15日)。中位PFS为16.8个月(95%CI:9.2~NR),6个月PFS率为78.3%。6个月OS率为95.0%。
在安全性方面,53例患者中有52例经历了与治疗相关的不良事件(TRAE),但其中92%事件为1级和2级。最常见的TRAE(≥30%)为贫血(75.5%) ),疲劳(67.9%),手足综合征(52.8%),腹泻(45.3%),高血压(43.4%),恶心(35.8%)和ALT / AST升高(32-34%)。 ≥5%的受试者经历的3级TRAE为高血压(22.4%),贫血(11.3%),疲劳(11.3%)和ALT升高(5.7%)。 两名受试者经历了3级缺氧。 没有发生4级TRAE或死亡。 TRAEs导致6名受试者(11.3%)停用belzutifan和8名受试者(15.1%)停用cabozantinib。
在这项初步分析中,belzutifan联合卡博替尼在转移性ccRCC患者的后线治疗中显示出了良好的抗肿瘤活性。安全性与预期一致。虽然,队列2仍然在进一步随访观察,队列1(以前未经治疗的ccRCC患者)的数据还在待待中。但令人欣喜的是,在控制下游信号传导的转录因子水平上靶向假性低氧的机制病理生理也是可以靶向的(例如带有卡博替尼的VEGFRs)。 未来必须包括对可能对这些疗法有抗药性(或产生抗药性)的受试者进行评估,并在头对头研究中进行比较。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ASC#
0
#透明细胞癌#
40
#细胞癌#
39
#抑制剂#
31
#HIF#
33
希望进展有效。
89
谢谢梅斯提供这么好的信息,学到很多
57