CLIN CANCER RES:Iniparib联合同步放化疗治疗胶质母细胞瘤
2019-01-20 MedSci MedSci原创
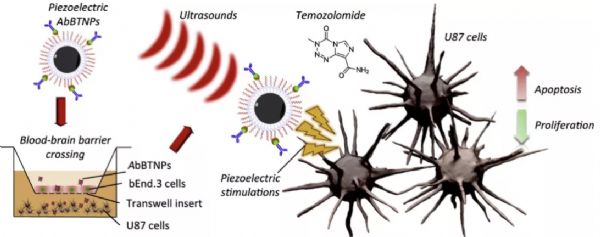
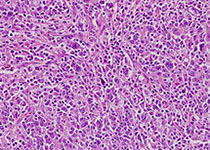
Iniparib在胞内转化为硝基自由基离子导致细胞死亡,是一种前药,CLIN CANCER RES近期发表了一篇文章,评估iniparib联合标准放疗和替莫唑胺治疗新诊断的胶质母细胞瘤(GBM)患者的疗效和安全性。
Iniparib在胞内转化为硝基自由基离子导致细胞死亡,是一种前药,CLIN CANCER RES近期发表了一篇文章,评估iniparib联合标准放疗和替莫唑胺治疗新诊断的胶质母细胞瘤(GBM)患者的疗效和安全性。
该试验为前瞻性多中心 II期试验,与历史对照组比较中位总生存期(mOS)的情况。放射治疗+替莫唑胺+ iniparib(n = 5)的安全性验证研究后进行功效研究(n = 76),使用iniparib的推荐II期剂量(8.0 mg / kg静脉注射 每周两次联合放疗+每日替莫唑胺治疗,续贯8.6mg / kg每周两次联合每次5天的替莫唑胺治疗,28天周期)。研究结最终纳入81名患者,中位年龄为58岁(男性为63%)。87%的患者者基线KPS≥80%。mOS为22个月。2年和3年生存率分别为38%和25%。27%的患者出现治疗相关的3级不良事件(AEs); 9名患者需要停药,AE包括输液相关反应,皮疹,胃炎,肝酶升高和血小板减少症。
原始出处:
Jaishri O. Blakeley, Stuart A. Grossman, et al. Phase II Study of Iniparib with Concurrent Chemoradiation in Patients with Newly Diagnosed Glioblastoma. CLIN CANCER RES. January 2019 doi: 10.1158/1078-0432.CCR-18-0110
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胶质母细胞#
22
#母细胞瘤#
29
#Iniparib#
26
#放化疗#
28
#细胞瘤#
31
#同步放化疗#
36