JACC:重度主动脉狭窄患者经导管主动脉瓣置换术后2年的预后
2021-03-07 MedSci原创 MedSci原创
经导管主动脉瓣置换术治疗重度主动脉狭窄的2年预后是否仍明显优于手术治疗?
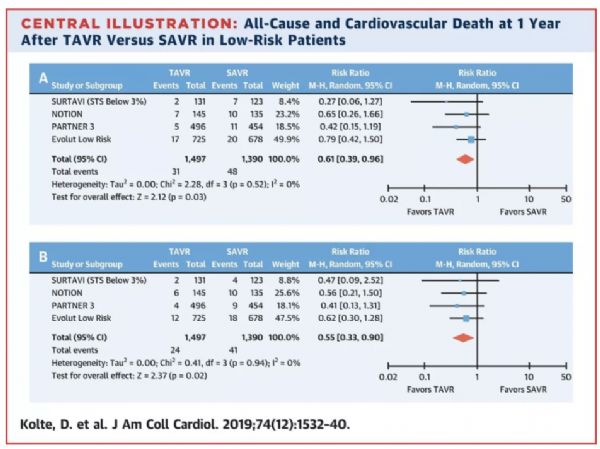
PARTNER 3试验显示,低手术风险的有症状的重度主动脉瓣狭窄患者,经导管主动脉瓣置换术(TAVR)治疗的1年后死亡、中风或再次住院的主要终点均经优于手术治疗。
本次分析旨在评估PARTNER 3试验患者治疗后1到2年内的临床和超声心动图结果。
共有1000名患者按1:1随机接受SAPIEN 3瓣膜经股动脉TAVR或手术治疗。术后30天、1年和2年时对患者进行临床和超声心动图检查随访。本次分析评估了主要终点和几个次要终点(临床、超声心动图和生活质量测量)的2年发生率。
主要终点
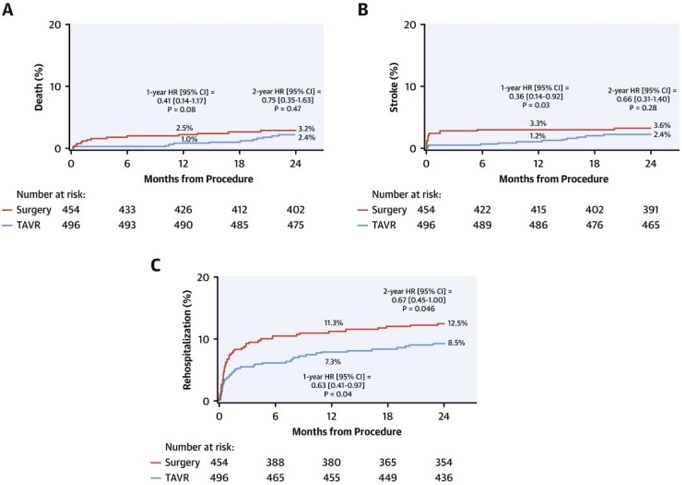
96.5%的患者获得了2年的主要终点随访。TAVR组术后2年的主要终点发生率与手术组相比显著降低(11.5% vs 17.4%;风险比:0.63;95%CI:0.45-0.88;p=0.007)。在2年时,两组间的死亡和中风发生率差异没有统计学意义(TAVR vs 手术:死亡 2.4% vs 3.2%,P=0.47;中风 2.4% vs 3.6%,P=0.28)。
超声心动图:血流动力学表现
TAVR术后2年的瓣膜血栓形成率高于手术(2.6% vs 0.7%;P=0.02)。TAVR治疗2年后,疾病特定性的健康状况继续优于手术治疗。两组治疗后2年内的超声心动图结果,包括血流动力学瓣膜恶化和生物瓣膜衰竭,均无明显差异。
总之,对于有症状的重度主动脉瓣狭窄患者,采用TAVR治疗后2年内的主要终点发生率始终低于手术治疗的低,但两组间的死亡和卒中的初始差异减小,且接受TAVR治疗的患者的瓣膜血栓发生率增加了。
原始出处:
Leon Martin B,Mack Michael J,Hahn Rebecca T et al. Outcomes 2 Years After Transcatheter Aortic Valve Replacement in Patients at Low Surgical Risk. J Am Coll Cardiol, 2021, 77: 1149-1161.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JACC#
23
#置换#
24
世间哪得双全法
69
#主动脉狭窄#
35
#ACC#
27
#主动脉瓣#
26
#主动脉瓣置换术#
26
#主动脉#
31
#动脉狭窄#
32
#经导管#
35