Liver Cancer:卡瑞利珠单抗(Camrelizumab)治疗既往治疗进展的晚期肝细胞癌(HCC)患者的疗效:2期临床研究长期随访结果更新
2021-07-01 yd2015 MedSci原创
长期随访进一步证实,卡瑞利珠单抗(Camrelizumab)可以改善既往治疗进展的晚期肝细胞癌(HCC)患者的预后。
免疫治疗的发展为晚期肝细胞癌(HCC)患者提供了更多的治疗选择。根据2期CheckMate-040和KEYNOTE-224研究的结果,nivolumab和pembrolizumab在美国被批准用于既往接受索拉非尼治疗的晚期肝癌患者。在III期临床研究CheckMate-459中,nivolumab与sorafenib作为晚期HCC的一线治疗方法进行了比较。虽然nivolumab的总生存期(OS)没有达到统计学意义,但可以观察到nivolumab治疗有OS、客观缓解率(ORR)和完全缓解率获益倾向。
卡瑞利珠单抗(Camrelizumab)是我国自主研发的PD-1抑制剂。2020年在Lancet Oncol杂志上发表了我国任正刚教授开展的II期临床研究结果,证实在中国晚期肝癌患者中,治疗后进展应用卡瑞利珠单抗可改善患者的预后。在12.5个月的中位随访中,接受卡瑞利珠单抗治疗患者的ORR为14.7%(95% [CI] 10.3 20.2),中位应答持续时间(DoR)未达到;6个月的OS率为74.4% (95% CI 68.079.7),中位OS未达到。基于研究结果,卡瑞利珠单抗(Camrelizumab)在中国被批准用于索拉非尼或化疗进展后的晚期肝细胞癌(HCC)患者。近期,Liver Cancer杂志上发表了长期随访的更新结果。
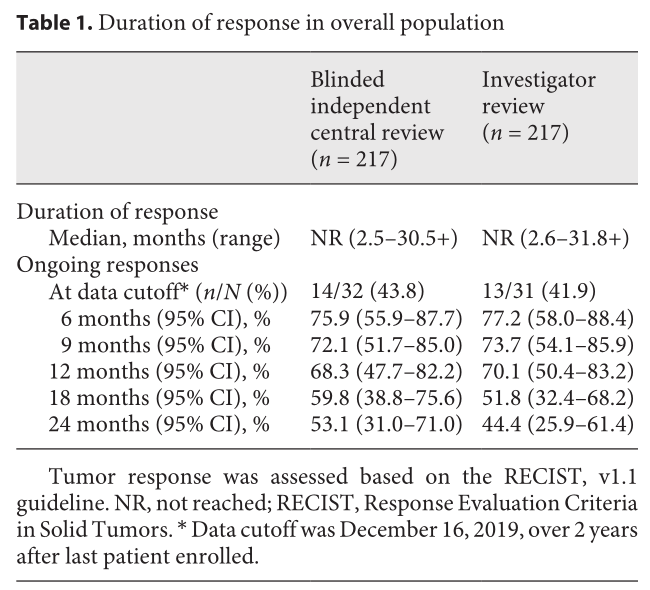
2016年11月15日至2017年11月16日,共有217例患者入组并接受至少1疗程camrelizumab: 其中109例每2周组,108例每3周组。截至2019年12月16日数据截止时,中位随访时间为13.2个月(IQR 5.7-25.8)。20例没有疾病进展的患者继续接受治疗。独立盲法评估委员会(BICR)评估有客观反应的32例患者中, 14例(43.8%)仍在持续应答中。6个月、12个月、18个月和24个月的持续反应率为75.9% (95% CI 55.9 - 87.7)、68.3% (95% CI 47.7 -82.2), 59.8% (95% CI 38.8 - 75.6)和53.1%(95%CI 31.0 - 71.0)。研究者评估DoR与BICR评估的一致。
疗效评估
截止数据,217例患者中146例(67.3%)死亡,中位OS为14.2个月(95% CI 11.5 16.3)。12个月、18个月和24个月的OS率分别为55.9% (95% CI 49.0 62.3)、41.3% (95% CI 34.6 47.9)和33.7% (95% CI 27.3 40.2)。

OS
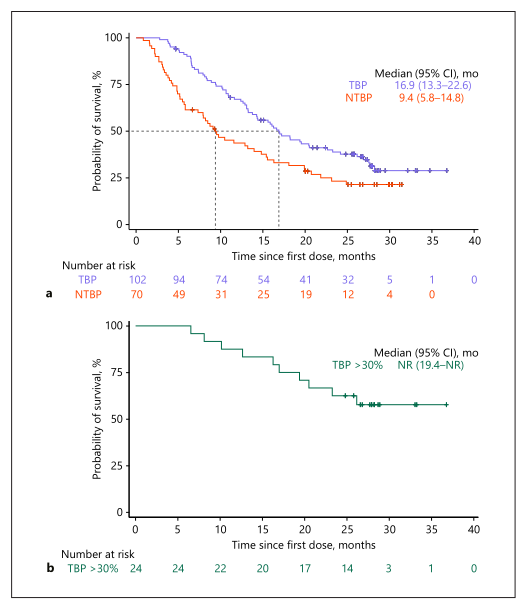
在172例(79.3%)接受RECIST标准评估的疾病进展(PD)患者中,102例(59.3%)继续接受cam- relizumab治疗(TBP组),而70例(40.7%)未接受治疗(非TBP组)。TBP组的中位OS为16.9个月(95% CI 13.3 22.6),而非TBP组为9.4个月(95% CI 5.8 14.8)。TBP组和非TBP组6、12、18和24个月 OS率分别为91.1% (95% CI 83.6–95.3) versus 61.4% (95% CI 49.0–71.7), 67.1% (95% CI 56.9–75.3) versus 43.7% (95% CI 31.8–54.9), 47.5% (95% CI 37.3–56.9) versus 33.1% (95% CI 22.3–44.3), 和38.8% (95% CI 29.2–48.4) versus 23.2% (95% CI 13.8–34.1)。
102例TBP组患者中有24例患者肿瘤较基线缩小大于30%,其中位OS未达到(95% CI 19.4未达到),6个月、12个月、18个月和24个月OS率分别为100% (95% CI未达到)、87.5% (95% CI 66.1 95.8)、75.0% (95% CI 52.6 87.9)和62.5% (95% CI 40.3 78.4)。
TBP和非TBP组的OS
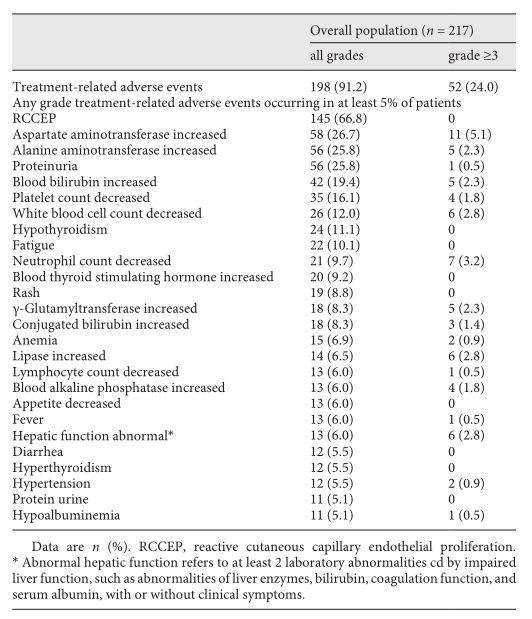
217例患者中198例(91.2%)发生至少1例治疗相关不良事件(TRAE), 3级及以上TRAE的发生率为24.0%(52例)。最常见的TRAE为毛细血管增生症(RCCEP)(66.8%),但均为1级或2级。其他常见不良事件包括天冬氨酸氨基转移酶升高(11例[5.1%]),中性粒细胞减少(7例[3.2%]),白细胞计数下降(6例[2.8%]),脂肪酶升高(6例[2.8%]),丙氨酸转氨酶升高(5例[2.3%]),γ-谷氨酰转移酶升高(5例[2.3%])血胆红素升高(5例[2.3%])。26例(12.0%)患者发生与治疗相关的严重不良事件。最常见的是肝功能异常(5例[2.3%]),且均为3或4级。TRAEs导致38例(17.5%)患者中断治疗,8例(3.7%)患者停止治疗。在长期随访期间,没有因TRAE导致的死亡。
不良事件
综上,长期随访进一步证实,卡瑞利珠单抗(Camrelizumab)可以改善既往治疗进展的晚期肝细胞癌(HCC)患者的预后。对于卡瑞利珠单抗治疗第一次评估进展(RECIST标准)的患者,继续卡瑞利珠单抗仍有生存获益。
原始出处:
Zhenggang Ren, Shukui Qin, Zhiqiang Meng, et al. A Phase 2 Study of Camrelizumab for Advanced Hepatocellular Carcinoma: Two-Year Outcomes and Continued Treatment beyond First RECIST-Defined Progression. Liver Cancer. DOI: 10.1159/000516470. Published online: June 30, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#camrelizumab#
32
#细胞癌#
30
#肝细胞#
36
#2期临床#
51
#MRE#
37
#CAM#
90
#随访结果#
46
#长期随访#
32
#mAb#
24
学习
48