Diabetologia:激活但功能受损的记忆Tregs在1型糖尿病患者进展缓慢的过程中逐渐扩展
2021-11-26 从医路漫漫 MedSci原创
从第一次出现胰岛自身抗体到出现1型糖尿病临床症状的进展率在儿童时期就有很好的描述,多个胰岛自身抗体阳性的儿童中有70%在血清转换后10年内患上糖尿病,而随访15年的儿童这一比例增加到84%。
从第一次出现胰岛自身抗体到出现1型糖尿病临床症状的进展率在儿童时期就有很好的描述,多个胰岛自身抗体阳性的儿童中有70%在血清转换后10年内患上糖尿病,而随访15年的儿童这一比例增加到84%。相比之下,占临床1型糖尿病一半以上的成人型1型糖尿病的发病机制还没有得到充分的研究。
越来越多的人开始使用分期系统来定义1型糖尿病的进展:个体在出现多种胰岛自身抗体时进入第1阶段,出现血糖异常时进入第2阶段,出现症状时进入第3阶段。一些多发胰岛自身抗体阳性的个体,在1期和2期,进展较慢,并发展为成人发病的1型糖尿病。我们之前描述了一组在首次检测到多种胰岛自身抗体样本后至少10年无糖尿病的极慢进展者,这组患者人数少,但特征非常明确。随后,我们发现胰岛自身抗原特异性CD8+T细胞反应在进展缓慢的患者中基本不存在,但在近期发病和长期存在的糖尿病患者中很容易检测到。这可能表明,与进展患者相比,这些患者自身免疫反应的调节增强。
早期研究表明,尽管调节性T细胞(Treg)数量正常,但糖尿病患者存在一些功能缺陷,其中包括对IL-2的反应能力降低。此外,糖尿病患者中的效应CD4+T细胞可能对调节更具抵抗性,表现为效应T细胞的抑制减弱,自然产生的Treg和体外产生的诱导Treg,以及抗原经历的CD4+T细胞中IL-2反应减弱。本研究的目的是描述了CD4+调节性T细胞(Treg)在一小群极缓慢进展者中的特征,他们的平均年龄为43岁(31-72岁),随访时间为18-32年。
方法:BOX研究是一项以人群为基础的纵向研究,在21岁以下确诊的患者亲属中检查1型糖尿病的危险因素。我们之前描述了长期缓慢进展者的特征,他们保持多重胰岛自身抗体阳性超过10年,但没有出现糖尿病的临床症状,慢性或非进行性自身免疫。随后,10名继续保持无糖尿病并愿意提供大量血液样本的缓慢进展者纳入T和B细胞功能分析。在目前的研究中,8名慢进展者(SP组),中位年龄43岁(31-72岁),18 - 32岁之间的胰岛自身抗体阳性。所有的参与者都处于1型糖尿病进展的1期,尽管一些人随后失去了胰岛自身抗体对某些抗原的阳性反应,然而,一名患者已经处于2期至少6年,但没有出现临床症状,一名患者被诊断为糖尿病,该受试者72岁,在采集实验样本时,其HbA1c升高到53 mmol/mol(7%),在数据分析中对该供体进行了单独评估。分离外周血单个核细胞(PBMCs),采用多参数流式细胞术和T细胞抑制试验评估供体中Treg的频率、表型和功能。使用FlowSOM和CITRUS(聚类鉴定、表征和回归)进行无监督聚类分析,评估Treg表型。
结果:与健康供体相比,来自慢进展体的记忆CD4+T细胞的监督聚类显示,激活的记忆CD4+ Treg频率增加,与糖皮质激素诱导的TNFR相关蛋白(GITR)表达增加有关。一名HbA1c升高的患者与进展缓慢者和匹配的对照组相比,Treg谱有所不同。功能分析表明,与健康供体相比,来自缓慢进展体的Treg介导的CD4+效应T细胞抑制明显受损。表现为对效应CD4+T细胞CD25和CD134表达的抑制增加。

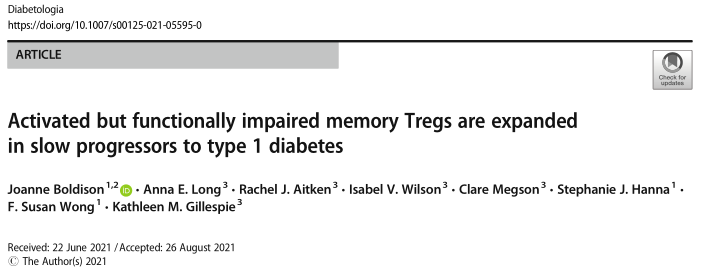
图1 深入的表型分析显示,CD4+Treg亚型在慢进展队列中增加。由FlowSOM生成的Treg室,聚集在来自所有供体的活CD4+CD45RA -细胞上。根据标记物表达鉴定出10个元簇:记忆T细胞_1;记忆T cell_2;记忆T cell_3;记忆T cell_4;CD49b记忆T细胞;HLA-DR + GITR +记忆T细胞;内存Treg_1;内存Treg_2;内存Treg_3;和内存Treg_4。(a)使用9个不同Treg标记生成的10个元簇的MST。每个节点代表一个集群(100个集群),更大的元集群(10个元集群)在节点组周围上色。每个节点中的饼图表示单个标记的表达级别。(b)每个元聚类的热图,以显示整体标记表达。(c, d)为HD组(c)和SP组(d)生成图,以及FlowSOM识别的每个元簇的覆盖层。(e-l)相对丰度为每个metacluster箱线图(丰度> 0.05%)确定为HD和SP组:内存Treg_2 (e),内存Treg_3 (f),内存Treg_4 (g), HLA-DR + GITR +记忆T细胞(h)、记忆T cell_1(i),记忆T cell_2 (j),记忆T cell_3 (k) n d CD49b记忆T细胞(l)。橙色圆点代表捐赠者SP 606。**p< 0.01, Wilcoxon配对符号秩检验。此键适用于图形部分(a), (c), (d)和d (e-l)
图2 使用CITRUS的预测模型证实,Treg频率的增加是进展缓慢的标志。分级门控(a - f)和柑橘分析(g-k)比较SP参与者和匹配的HD参与者在CD4+CD45RA−T细胞上的差异。(a)亲本CD25+ cd127 lotreg和CD25loCD127+T c e l群体的代表性图。CD25+ cd127lotreg被CD39和FOXP3富集,然后通过HLA-DR和GITR表达进行分离,模拟FlowSOM群体。(b) HD(黑点)和SP(蓝点)组以及供体SP 606(橙色)中CD25+ cd127的频率汇总图。(c-f) CD25+CD127loCD39+FOXP3+和CD25loCD127+门控子集的箱线图;(c) HLA-DRloGITR−(内存Treg_2), (d) HLA-DRintGITRlo(内存Treg_3), (e) HLA- d RhiGITR+(内存Treg_4), (f) HLA- d RhiGITR+(HLA-DR+GITR+内存T cell)。(g - i)柑桔簇螺旋由(g) CD127, (h) CD25和(i) FOXP3表达强度着色,箭头突出的簇被识别为SP和HD队列之间的不同。(j)箱线图显示了在SP(蓝点)和HD(灰点)组中,CITRUS记忆Treg_3和Treg_4的相对丰度(比例)。(k)直方图显示每个簇的表型(粉红色)和Treg标记相对表达与背景表达(蓝色);上列,内存Treg_3;下面一行,内存Treg_4。背景与所有其他簇中标记的表达有关。*p< 0.05, **p< 0.01, Wilcoxon配对符号秩检验

图3 与健康献血者相比,进展缓慢者记忆treg的GITR增加。每个记忆CD4+T细胞元簇(记忆T细胞_1;记忆T cell_2;记忆T cell_3;CD49b +记忆T细胞;HLA-DR + GITR +记忆T细胞;内存Treg_2;内存Treg_3;来自FlowSOM的memory Treg_4)检测每个表达标记的变化。(a,b)来自HD (a)和S (b)队列的表达热图(sp606不包括在内)。(c,d)记忆Treg_4元簇中所有HD(灰色)、所有SP(蓝色)和SP 606(橙色)的FlowSOM GITR表达串联,显示直方图(c)和汇总图(d)。Wilcoxon配对符号秩和检验,p< 0.07(橙色)所有供体包括,p< 0.05(蓝色)供体SP 606和匹配的HD不包括在测试中。(e,f) HLA-DRhiGITR+Tregs中GITR表达,从分级门控,从所有HD(灰色)、所有SP(蓝色)和SP 606(橙色)串联,显示直方图(e)和汇总图(f) *p< 0.05, Wilcoxon配对符号秩检验

图4 来自缓慢进展的CD4+ treg细胞控制效应CD4+T细胞的能力降低。SP组用蓝色的线和圆点表示,HD组用黑色的线和圆点表示,橙色的线/圆点表示供体sp606。使用CD4+CD25+ Treg分选试剂盒对CD4+T细胞进行分选。CD4+CD25−(应答者)被标记为CFSE, Treg按观察的比例滴定。用抗CD3 /28微珠活化细胞,培养3天后进行流式细胞术检测。(a-d)与CD4+应答者相对应的treg培养(自体)(e-h) HD、SP或SP 606 Treg与HD应答者培养。(a,b,f) CFSE增殖(a,e)和CFSE抑制百分比(b,f)。(c, d,h) CD25 (c,g)和CD134 (d,h)的抑制百分比。使用阳性对照(激活的响应细胞不含treg)计算抑制百分比。*p< 0.05, **p< 0.01, ***p< 0.001,重复测量双向方差分析。†p < 0.0 5 Bonferroni的事后多重比较测试

图5 效应CD4+T细胞对缓慢进展的T细胞活化的抑制更敏感。SP组用蓝色的线和圆点表示,HD组用黑色的线和圆点表示,橙色的线/圆点表示供体sp606。使用CD4+CD25+Treg分选试剂盒对CD4+T细胞进行分选。CD4+CD25−(应答者)被cfsel标记,treg按观察的比例滴定。用抗CD3 /28微珠活化细胞,培养3天后进行流式细胞术(CD25反染)和细胞因子分析。HD Treg与HD、SP或sp606应答者共同培养。(a,b) CFSE增殖(a)和CFSE抑制百分率(b)。(c,d) CD25抑制百分率(c)和CD134抑制百分率(d)。(e,f) IFN-γ(e)和IL-17A (f)在共培养中的表达。***p< 0.001, **p< 0.01,重复测量双向方差分析。†p < 0.0 5 Bonferroni的事后多重比较测试
结论:我们得出的结论是,来自缓慢进展子的活化记忆CD4+Treg在GITR表达中得到了扩展和丰富,强调了进一步研究Treg在1型糖尿病风险个体中的异质性的必要性。
原文出处:
Boldison J, Long AE, Aitken RJ,et al.Activated but functionally impaired memory Tregs are expanded in slow progressors to type 1 diabetes.Diabetologia 2021 Oct 28
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Tregs#
37
#BET#
28
#DIA#
34
#1型糖尿病患者#
33
您好,这些图能讲的详细点吗,没看懂。
36
学习了
48
#糖尿病患者#
18
#Treg#
28