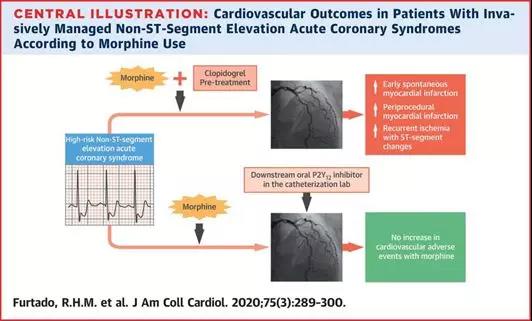
JACC: 吗啡和氯吡格雷不要同时用!增加ACS患者缺血事件风险
2020-01-26 朱朱 中国循环杂志
临床上,吗啡是缓解急性冠脉综合征胸痛的药物之一。但机制性研究显示,吗啡可能会影响口服抗血小板药物(二磷酸腺苷受体拮抗剂)的抗血小板效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
30
#ACS#
24
#ACC#
0
#吗啡#
42
#ACS患者#
42
学习了
85