Nature Communications:耶鲁大学研究,揭开血脑屏障分子机制,短暂打开血脑屏障
2022-03-21 王聪 “生物世界”公众号
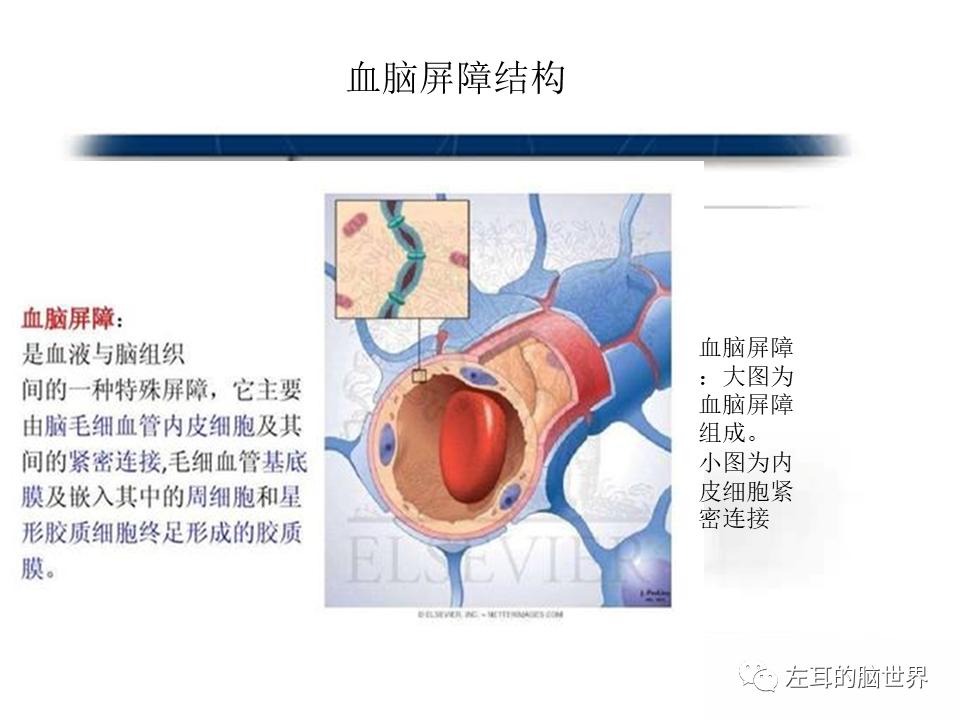
血脑屏障是指脑毛细血管壁与神经胶质细胞形成的血浆与脑细胞之间的屏障,和由脉络丛形成的血浆和脑脊液之间的屏障,仅允许特定类型的分子从血流进入大脑神经元和其他周围细胞。
我们人类最重要的器官——大脑,其中包含了数百亿个相互作用的神经元,它们非常重要而又十分脆弱,需要在特殊的保护环境下才能正常运作。血脑屏障(BBB)就是其重要的保护作用机制,
血脑屏障是指脑毛细血管壁与神经胶质细胞形成的血浆与脑细胞之间的屏障,和由脉络丛形成的血浆和脑脊液之间的屏障,仅允许特定类型的分子从血流进入大脑神经元和其他周围细胞。
血脑屏障的存在,对于阻止有害物质由血液进入大脑具有重要意义,然而,血脑屏障同时也阻止了绝大部分小分子和大分子(例如多肽,蛋白质和核酸)的转移,严重限制了中枢神经系统疾病(例如神经退行性疾病、脑肿瘤,脑部感染和中风等)的治疗。
因此,当一个人患上了中枢神经系统疾病,原本起保护作用的血脑屏障反而成了“最大的敌人”。一直以来,科学家们都想找到一种方法,来临时打开血脑屏障进行药物递送,然后在重新封上的方法。
近日,美国耶鲁大学的研究人员在 Nature Communications 期刊发表了题为:Endothelial Unc5B controls blood-brain barrier integrity 的研究论文。
该研究首次揭开了调控血脑屏障的分子机制,血管内皮细胞的受体Unc5B通过调控Wnt信号通路来维持血脑屏障的完整。通过抗体抑制Unc5B与其配体Netrin-1的结合,能够短暂打开血脑屏障,并在数小时候重新封上。这一发现为将来针对中枢神经系统的药物递送和治疗打开了新的大门。

血脑屏障的发育和维持依赖于所谓的Wnt信号通路,该通路调节许多关键的细胞过程,研究团队一直试图弄清楚是否可以调节这一信号通路以“按需”打开血脑屏障。
2017年,Kevin Boyé(该论文的第一作者)作为博士后加入了 Anne Eichmann(该论文的通讯作者)实验室,他开始研究Unc5B蛋白,这是一种毛细血管内皮细胞中表达的内皮膜受体蛋白。
他们发现,如果敲除小鼠的Unc5B基因,它们会在胚胎发育早期就死亡,死亡原因是脉管系统未能正常形成,这表明Unc5B是血管发育中的重要分子。他们还发现,一种名为Claudin5的蛋白也显着减少,而该蛋白内皮细胞之间建立血脑屏障非常重要。这些发现让研究团队意识到Unc5B在维持血脑屏障中起着重要作用。
在此之前,科学家们并不知道Unc5B和Wnt信号通路之间有什么联系,而在这项新研究中,他们发现Unc5B其实控制着Wnt信号通路,起着上游调节剂的作用。
接下来,研究团队在已经建立了血脑屏障的成年小鼠中敲除其Unc5B受体,发现小鼠的血脑屏障会打开。他们进一步找到了Unc5B受体的配体——Netrin-1,抑制该配体同样可以打开血脑屏障。
研究团队在此基础上,开发了一种抑制Netrin-1与Unc5B结合的抗体,静脉注射该抗体后,Wnt信号通路被破坏,进而导致血脑屏障暂时性打开。
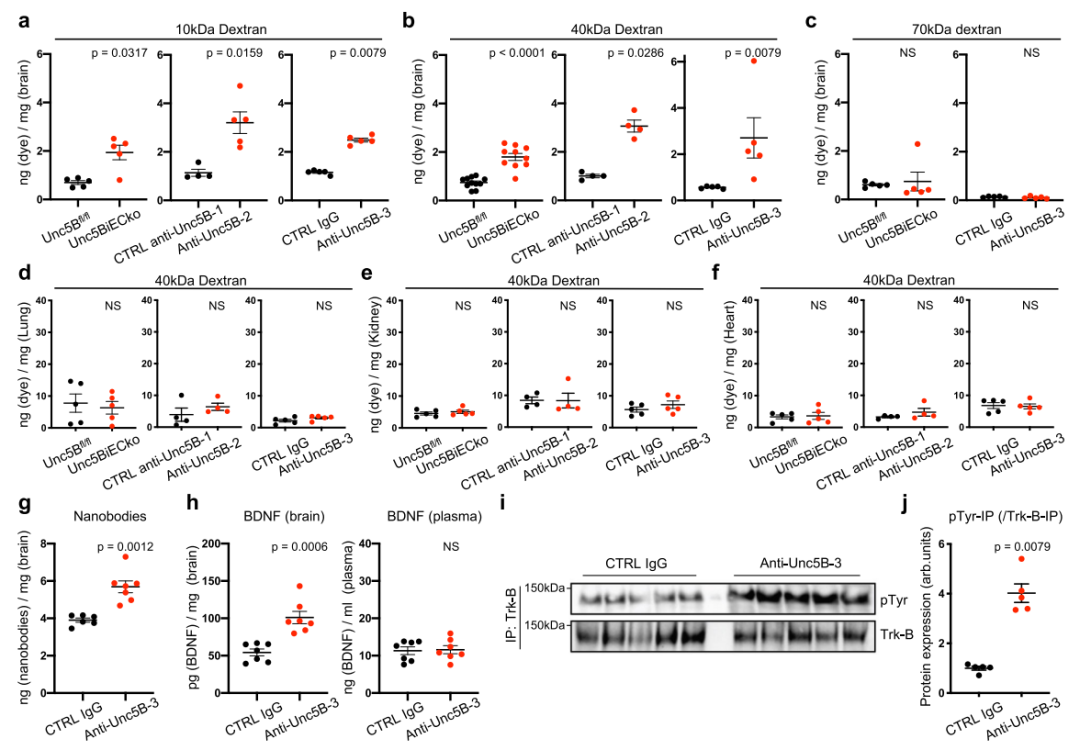
总的来说,该研究表明,血管内皮细胞受体Unc5B通过调控Wnt信号通路来维持血脑屏障的完整。在机制上,Unc5B的配体Netrin-1增强Unc5B与Wnt共受体LRP6的相互作用,诱导其磷酸化并激活Wnt/β-catenin下游信号转导。通过静脉内递送阻断Netrin-1与Unc5B结合的抗体,会导致短暂的Wnt信号转导中断和血脑屏障打开,几小时后血脑屏障会重新封上。
血脑屏障的存在阻止了绝大部分小分子和大分子进入大脑,因此,阿尔茨海默病、多发性硬化症、脑肿瘤、抑郁症等中枢神经系统疾病极难治疗。而这项研究首次揭开了调控血脑屏障的分子机制,从而可以针对性暂时打开血脑屏障,为将来针对中枢神经系统的药物递送和治疗打开了新的大门。
原始出处:
Boyé, K., Geraldo, L.H., Furtado, J. et al. Endothelial Unc5B controls blood-brain barrier integrity. Nat Commun 13, 1169 (2022). https://doi.org/10.1038/s41467-022-28785-9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
69
#Nat#
29
学习
56
#血脑屏障#
0
#Nature Communications#
50
学习学习了
51