Nat Med:COVID-19住院患者输注恢复期血浆的疗效
2021-09-10 MedSci原创 MedSci原创
对于COVID-19患者,与标准治疗相比,输注恢复期血浆可能会导致更差的临床结局。
恢复期血浆对2019冠状病毒病(COVID-19)的疗效尚未明确。尽管大多数随机对照试验都表现出负面结果,但非对照研究表明抗体含量可能会影响患者的预后。

近日,顶级医学期刊Nature Medicine上发表了一篇研究文章,研究人员对在呼吸道症状发作后12天内接受吸氧和恢复期血浆治疗的COVID-19成人中进行了一项开放标签、随机对照试验(NCT04348656)。患者按2:1被分配至500ml的恢复期血浆或标准治疗。该研究的复合主要结局是插管或30天死亡。研究人员在探索性分析中通过Logistic回归评估恢复期血浆抗体对主要结局的影响。
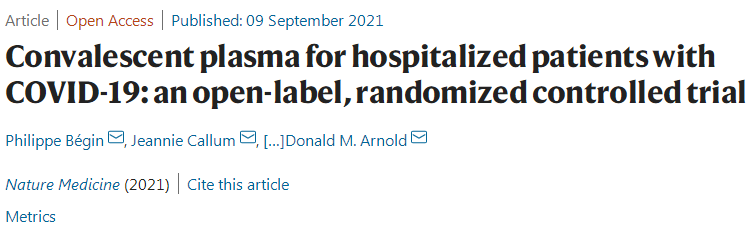
该研究总共纳入940名患者被随机分组,其中921名患者被纳入意向治疗分析。恢复期血浆组199/614(32.4%)名患者和标准治疗组86/307(28.0%)名患者接受插管或死亡—相对风险(RR)=1.16(95%置信区间(CI)0.94–1.43,P=0.18)。恢复期血浆组的患者有更严重的不良事件(33.4% vs. 26.4%;RR=1.27,95%CI为1.02–1.57,P=0.034)。抗体含量显著调节了恢复期血浆的治疗效果。
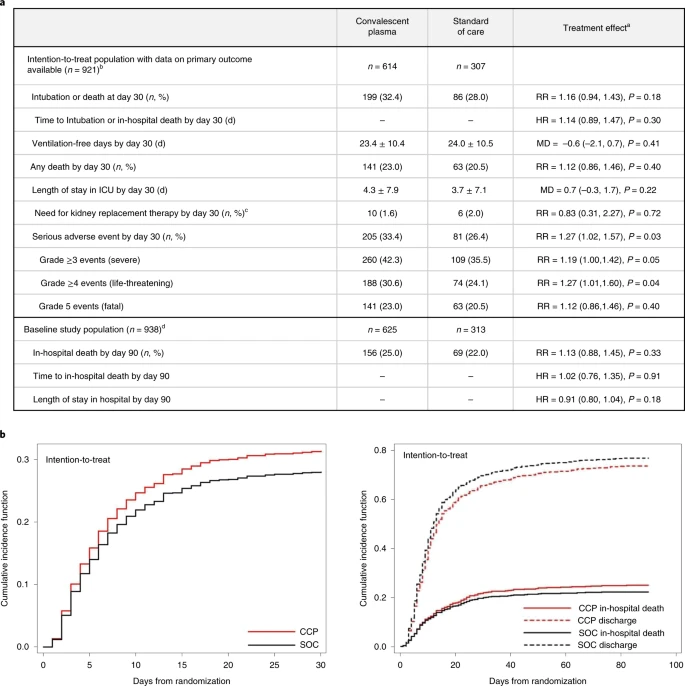
在多变量分析中,中和或抗体依赖性细胞毒性的每个标准化对数增加可降低血浆的潜在有害影响(比值比(OR)=0.74,95%CI为0.57–0.95和OR=0.66,95%CI为0.50–0.87),而针对全跨膜刺突蛋白的IgG增加了有害效应(OR=1.53,95%CI为1.14–2.05)。恢复期血浆并未降低住院COVID-19患者30天时插管或死亡的风险。
由此可见,对于COVID-19患者,与标准治疗相比,输注恢复期血浆可能会导致更差的临床结局。
原始出处:
Philippe Bégin,et al.Convalescent plasma for hospitalized patients with COVID-19: an open-label, randomized controlled trial.Nature Medicine.2021.https://www.nature.com/articles/s41591-021-01488-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#恢复期#
40
#Nat#
28
#恢复期血浆#
24
#Med#
21
挺好
47
不错
44
嗯我论文阿扣咯咯咯,?…
41
谢谢梅斯提供这么好的信息,学到很多
45