Nature:突破!单克隆抗体或有望治疗冠心病!
2018-06-10 Michael,Zoe 转化医学网
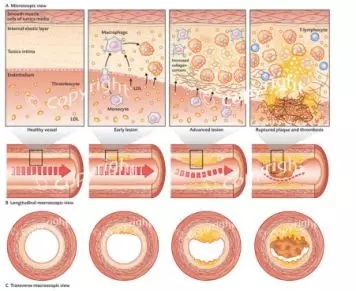
加利福尼亚大学圣地亚哥分校医学院的研究人员发现,抗氧化磷脂(OxPL)抗体通过与细胞表的氧化磷脂(OxPL)结合,不仅可以阻断小鼠体内的炎症反应, 即使在高脂饮食中,抗体还能保护小鼠免受动脉斑块形成,动脉硬化和肝脏疾病的侵袭,并延长其寿命。这篇文章发表于近日的《Nature》杂志。
导 读
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#克隆#
41
#Nat#
45
很好的学习机会
90
学习了谢谢
84
冠心病治疗新突破.学习了.
88
了解一下.谢谢分享!
81
值得期待啊
80