防控有道,风险管理丨黄幸涛:早发冠心病患者的PCSK9i应用经验
2021-07-02 “心关注”公众号 “心关注”公众号
哈尔滨医科大学附属第二医院黄幸涛医师分享了1例早发冠心病患者使用PCSK9抑制剂控制血脂水平,逆转斑块狭窄的的病例。患者为年轻男性,因阵发性胸痛1周,加重3天入院。
哈尔滨医科大学附属第二医院黄幸涛医师分享了1例早发冠心病患者使用PCSK9抑制剂控制血脂水平,逆转斑块狭窄的的病例。患者为年轻男性,因阵发性胸痛1周,加重3天入院。患者既往有高脂血症且吸烟,属于ASCVD极高危患者。在接受PCSK9抑制剂依洛尤单抗治疗后,患者LDL-C显着下降,迅速实现<1.4 mmol/L,降幅≥50%的目标,且LDL-C长期维持低水平状态。冠脉狭窄也明显逆转,症状减轻。特邀哈尔滨医科大学附属第一医院杨树森教授对病例进行点评,充分肯定了PCSK9抑制剂在降低血脂,缩小斑块面积方面的有效性、合理性和必要性,并表示尽早且持续使用PSCK9抑制剂可为患者带来更多获益,并可改逆转斑块进展,降低心脑血管事件发生风险。
病史资料:第一次入院
患者信息:37岁,男性
入院时间:2019年10月
主诉:阵发性胸痛1周,加重3天。
现病史:患者于入院前1周于快步行走后出现阵发性胸闷,伴咽部紧缩感,持续10-20分钟后缓解,未向背部、上肢等部位放射,平均每日发作1次,性质、部位、持续时间同前,多于每日外出,早晨时发作,3日前再次出现发作性胸闷及咽部紧缩感,程度较前明显加重,发作时无法继续行走,于当地医院就诊并行造影检查,自述结果回报冠脉狭窄约 90%,未支架,静点改善循环药物(具体名不详),未见明显好转,现求明确诊治于今日来我院就诊。
既往史:否认高血压、高血脂、糖尿病病史。
个人史:无。
家族史:无。
体格检查:36.6℃ 脉搏:79次/分 呼吸:18次/分 血压:128/76mmHg BMI:24.9。神清语明,一般良好,步入病室。心率:79/分各瓣膜区未闻及杂音 双肺无啰音 腹软,无压痛反跳痛。无皮疹,浅表淋巴结无肿大,巩膜无黄染,双下肢无浮肿。
辅助检查:
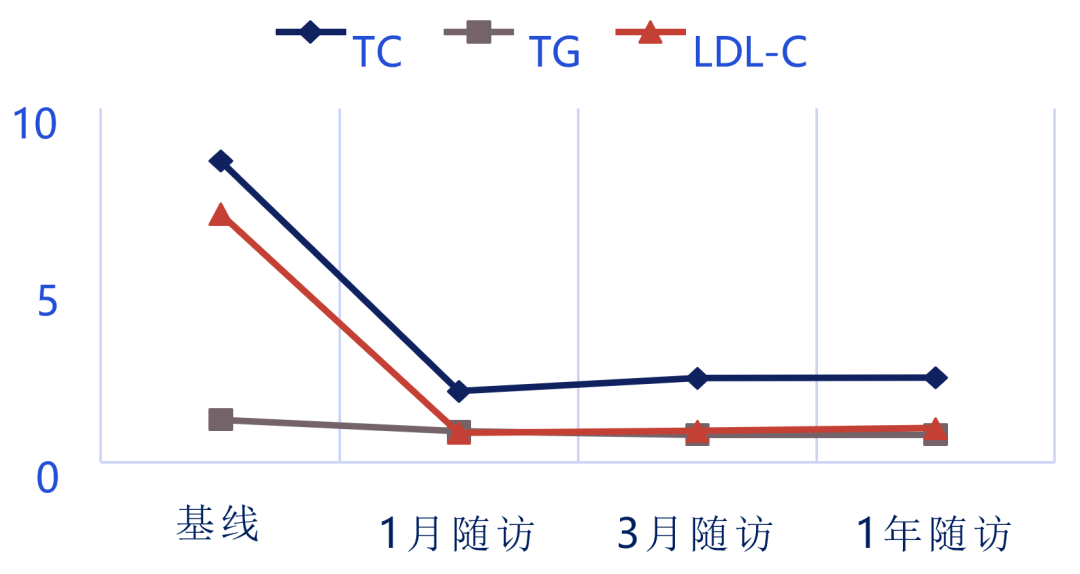
- 血脂:总胆固醇CHOL 8.53mmol/L↑,甘油三酯TG1.21mmol/L,高密度胆固醇HDL-c 0.82mmol/L↓, 低密度胆固醇LDL-c 7.02mmol/L↑,apoB:2.17mmol/L↑。
- 心肌酶谱:未见异常
- 肝肾功能离子:未见异常
- 血尿常规: 未见异常
- 血糖相关:糖化血红蛋白:5.70%
- 心脏彩超:左心房内径34.8mm,右心房内径 37.2×40.2mm,左心室舒末内径41.8mm,室间隔厚度9.5mm,左室后壁厚度9.6mm,左室后壁振幅10.0mm,EF:70%。提示:1.左心室壁向心收缩尚协调,2.三尖瓣轻度反流,3.左心功能正常。
诊疗方案
入院诊断:- 冠状动脉粥样硬化性心脏病
- 不稳定型心绞痛
- 高脂血症
治疗经过 :入院后,分析病情,给与阿司匹林肠溶片、氯吡格雷抗血小板,阿托伐他汀降血脂,琥珀酸美托洛尔控制心率,单硝酸异山梨酯缓解症状,灯盏细辛改善循环等治疗。并行冠状动脉造影检查。

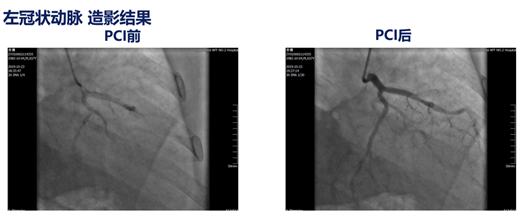
冠脉造影提示存在多支病变,行支架植入术。根据美国临床内分泌医师学会(AACE)和美国内分泌协会(ACE)发布的血脂管理和心血管病预防的新规则:极高危患者在生活方式+高剂量他汀的治疗下,LDL-C仍>55mg/dl时,使用PCSK9i应优先于依折麦布。极高危患者包括:进展性ASCVD(包括不稳定性心绞痛);确诊心血管病并伴糖尿 病或3-4期慢性肾病(CKD)或伴杂合子型家族性高胆固醇血症;早发心血管病(男性55岁前或女性65岁前确诊)。此患者考虑为极高危患者,血脂水平过高,预计他汀联合依折麦布无法使血脂水平达标,且患者经济条件许可,因此出院时调整降脂方案为阿托伐他汀+PCSK9抑制剂依洛尤单抗,拟1、3、6个月行门诊随访,1年时行造影复查。
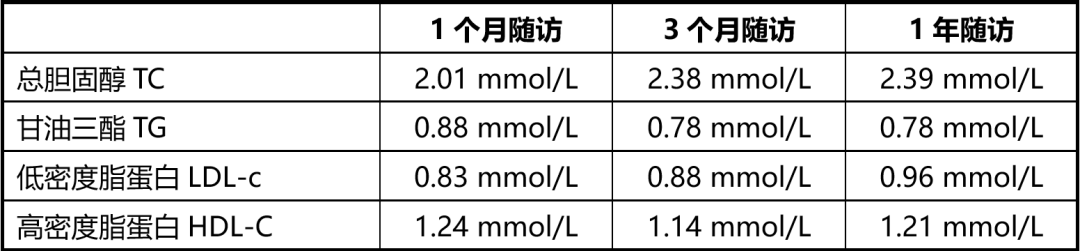
随访期间,血脂水平变化如下表:
复查冠脉造影,提示病变逆转。

PCSK9抑制剂用药理由
PCSK9抑制剂用药理由:
2019 ESC/EAS血脂异常管理指南推荐,极高危患者的LDL-C应较基线降低≥50%且LDL-C目标值<1.4mmol/L(<55mg/dL)(Ia类推荐);对于尽管使用最大耐受剂量他汀联合依折麦布治疗LDL-C仍未达标的ACS患者,在事件发生后早期(如果可以,在因ACS住院期间)应考虑联合PCSK9抑制剂(Ⅱa类推荐)。而美国临床内分泌医师学会(AACE)和美国内分泌协会(ACE)血脂管理和心血管病预防共识提出了降脂的新规则:在进一步降低LDL-C方面,不建议在给予他汀类药物后给予依折麦布,而是如果患者风险极高,估计加用依折麦布不能使LDL-C低于55 mg/dl, 则应直接应用PCSK9抑制剂,然后才加依折麦布或其他药物。
既往多项研究已经证实,依洛尤单抗在他汀基础上进一步降低LDL-C水平达59-75%。且研究显示,在他汀基础上联合依洛尤单抗治疗3个月,可促进ACS患者脂质斑块的逆转和纤维帽厚度增加。GLAGOV研究也表明,与安慰剂相比,在他汀治疗基础上使用依洛尤单抗治疗,在78周观察到显着逆转冠脉斑块。结合指南和临床试验研究,对于ASCVD患者,依洛优单抗注射液应尽早使用,低密度胆固醇迅速达标,可显着逆转斑块。使患者的心血管获益随时间不断增加,从而取得满意的治疗效果。
PCSK9抑制剂使用方法:PCSK9抑制剂依洛尤单抗注射液140 mg/次,皮下注射;2周1次,出院后持续使用。
病例小结
黄幸涛 医学博士,主治医师,中华医学会成员,黑龙江省医疗保健国际交流促进会血栓与肺血管病专业委员会委员。
哈尔滨医科大学附属第二医院心血管内科,具有丰富的临床工作经验,擅长心血管内科各类疾病如冠心病、高血压、心功能不全及各种心律失常诊疗。目前主要从事冠心病动脉粥样硬化机制研究及OCT易损斑块检测的基础和临床研究工作。主持国家自然科学基金青年基金1项,主持中国博士后科学基金面上资助一等资助1项,黑龙江省博士后科学基金面上资助一等资助1项;参与国家自然科学基金项目4项,省级课题1项。发表SCI论文15篇,其中第一作者4篇。
本例患者为年轻男性,具有吸烟、高血脂等心血管危险因素。此次因早发冠心病入院,冠脉造影提示多支血管病变。属于ASCVD极高危患者。他汀治疗后患者血脂水平仍明显增高,在接受PCSK9抑制剂依洛尤单抗联合治疗后,患者LDL-C显着下降,迅速实现<1.4 mmol/L,降幅≥50%的目标,且LDL-C持续维持在较低水平,安全性良好。随访1年无MACE,复查冠脉造影提示病变有所逆转。
ACS患者常有数个非罪犯斑块,这些斑块在接受他汀等药物治疗后仍不断进展,导致管腔狭窄加重。事实上,非罪犯斑块正是ACS患者未来事件高发的重要原因之一。LDL-C升高是动脉粥样硬化斑块进展和破裂的核心机制,只有将LDL-C进一步降低,才有可 能进一步逆转斑块、降低事件。2019ESC/EAS指南提出了更低的LDL-C目标值,对ACS患者的降脂达标提出了更高的要求。在ACS患者中早期使用依洛尤单抗,可显着提高ACS患者LDL-C达标率,还可稳定及逆转冠脉斑块,且患者的心血管获益随时间不断增加,同时安全性和耐受性良好,受到 2019ESC/EAS指南的最高类别推荐(ⅠA)。
图片专家点评

点评专家:杨树森教授
杨树森,医学博士,博士后,教授,主任医师,博士研究生导师。哈尔滨医科大学附属第一医院心内科一病房主任。中国医师协会心脏重症专业委员会常务委员。黑龙江省医师协会心脏重症分会主任委员。美国心血管造影和介入学会(SCAI)委员。中华医学会心血管病学分会冠脉介入学组委员。黑龙江省医学会心血管内科专业委员会副主任委员。黑龙江省中西医结合学会心脏重症分会副主任委员。黑龙江省医协会常务理事。哈尔滨市医学会心血管内科专业委员会副主任委员。哈尔滨市医学会理事。中国老年保健医学研究会老年心血管病分会常务委员。中国医疗保健国际交流促进会胸痛分会常务委员。中国医师协会整合医学分会第一届委员会整合心血管病专业委员会委员。中国医学装备协会心血管装备技术专业委员会委员。世界中医药学会联合会介入心脏病专业委员会理事。海峡两岸医药卫生交流协会心血管专业委员会委员。卫生部心血管疾病介入诊疗培训基地(冠心病介入)导师。《中国急救医学》杂志编委,《中国医学前沿杂志(电子版)》编委。从事冠心病的基础研究与临床诊治工作,尤其侧重冠心病介入治疗。
本例患者为年轻男性,具有吸烟、高血脂等心血管危险因素。冠脉造影显示冠脉多处狭窄,给予支架植入治疗。根据ASCVD的危险分层,该患者属于ASCVD的极高危人群,对于血脂的控制应该更为严格。该患者入院时总胆固醇CHOL8.53mmol/L,低密度胆固醇LDL-c7.02mmol/L,远远高于ESC/EAS血脂异常管理指南推荐的目标值。考虑患者起始治疗及靶目标值的差距很大,即使给予最大剂量的他汀治疗及联合依折麦布治疗,患者的血脂很难达到目标值。从该角度出发给予PCSK9抑制剂依洛尤单抗治疗,经过一年的随访,患者的LDL始终处于指南推荐值,从影像学上患者的动脉硬化斑块也出现了逆转。整个治疗过程患者未述及不良反应。根据超高危动脉粥样硬化心血管基本患者血脂管理共识,所有超高危ASCVD人群,应在控制饮食和改善生活方式的基础上,尽早开始并长期进行降脂治疗。降脂治疗方案包括他汀类药物、依折麦布、PCSK9抑制剂等单药或联合治疗。根据LDL-C水平的干预靶标以及超高危ASCVD患者的血脂管理路径,临床医生需识别超高危ASCVD患者,选择合理的降脂治疗,达到血脂管理及预防不良心血管事件再发的目标。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#早发#
30
#PCS#
57
#Csk#
34
#冠心病患者#
38
#风险管理#
42
好病例
67