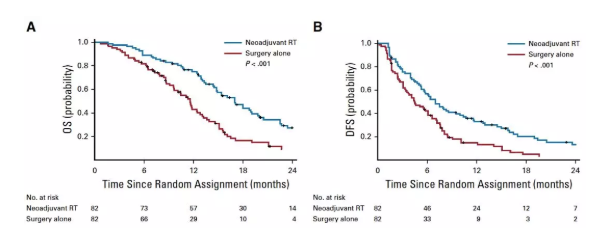
JCO:东方肝胆外科医院程树群教授团队发文:三维适形新辅助放疗显著改善可切除HCC伴PVTT患者的OS
2019-07-10 Lisa 肿瘤资讯
门静脉癌栓(PVTT)是肝细胞癌(HCC)预后较差的重要因素之一。BCLC分期系统推荐索拉非尼作为这类患者的唯一治疗策略。既往的一项回顾性分析显示,新辅助放疗可以降低部分HCC患者PVTT的侵犯范围,改善术后生存。由上海东方肝胆外科医院程树群教授牵头进行的一项多中心前瞻性随机研究,在HCC伴PVTT患者中前瞻性评估了新辅助放疗的价值,研究结果于7月8日在线发表于Journal of Clinica
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PVT#
33
#JCO#
27
#新辅助放疗#
0
#新辅助#
25
#肝胆外科#
36
#HCC#
22
#辅助放疗#
47
学习了
74
学习学习学习
73
好
83