Alzheimers Dementia:白质高信号病变分布特点不同,预测认知能力的效果也不同
2021-08-12 Freeman MedSci原创
WMH是导致AD患者认知能力下降的主要原因,与淀粉样蛋白沉积和萎缩无关
白质 高信号(WMH),在没有认知障碍的老年人中经常出现。它们与血管危险因素(VRF)有关,例如高血压或糖尿病,以及与较差的认知表现,特别是执行功能和处理速度有关。
在阿尔茨海默病(AD)患者中,WMH的体积似乎比认知障碍的老年人更大,特别是在脑室周围和后部区域。这些区域包括顶枕部和胼胝体压部(splenium of the corpus callosum,S-CC)。
AD和脑血管疾病有共同的VRF,并且经常并存。脑血管病变,如WMH,部分是由于小血管疾病,与临床AD的风险增加有关。它们可能会增加AD病变(即淀粉样蛋白沉积和神经纤维缠结),因此降低了认知障碍的阈值,或直接促进了AD的发生。
评估AD中WMH和认知之间关系的研究很少,研究结果也不一致。最近的一项荟萃分析显示,在所有主要的认知领域,WMH与AD患者的认知之间存在小到中等规模的关联,对注意力和执行功能的影响较大。
然而,人们对这些关联的区域特异性知之甚少,因为大多数AD研究分析的是全局WMH体积或脑室周围与深层WMH,但很少分析脑叶WMH。这一点尤其重要,因为WMH的空间分布似乎与部分不同的病因有关。
事实上,虽然大脑前部WMH与生理性衰老和VRF有关,但后部WMH与AD的关系更为特殊。此外,与深部WMH相比,脑室周围的WMH似乎与认知能力的恶化有更大的关联。
最后,研究还显示,与总的WMH负担相比,核心(strategic)白质束中的WMH与认知有更强的联系,如forceps minor或丘脑前部辐射。作为另一个警告,以前的WMH研究主要使用临床标准来诊断AD,没有包括生物标志物,这可能导致临床误诊,特别是在AD和血管性痴呆之间。仍然需要使用基于生物标志物的AD定义对AD背景下的WMH进行研究。
问题是,AD中WMH的数量和空间分布是否与年龄相关的WMH不同,以及WMH是否对Aβ阳性AD患者的认知有区域特异性影响。
藉此,法国诺曼底大学Antoine Garnier-Crussard1等人,探究了:
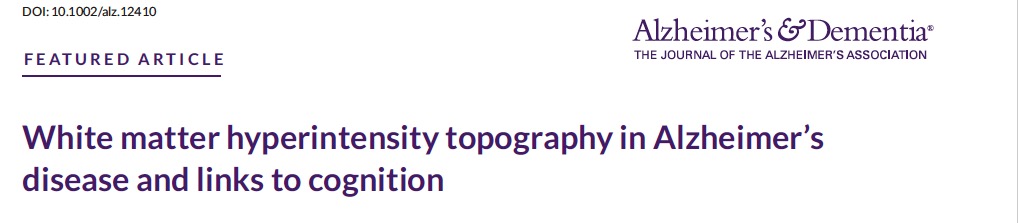
(1)通过与VRF匹配的Aβ阴性对照组(Aβneg-controls)进行比较,探究Aβ阳性的AD临床综合征患者(Aβpos-AD)的WMH的区域分布。
(2)评估区域WMH和认知表现之间的具体关系,并研究在控制了皮质淀粉样蛋白负担、海马和总灰质体积后,这些关系是否仍然存在。
他们对54名认知障碍的淀粉样β阳性AD(Aβpos-AD)的区域WMH进行估计,并与40名认知无障碍的淀粉样β阴性老年对照组(Aβneg-controls)进行血管危险因素匹配。在控制了大脑淀粉样蛋白负担、整体皮质萎缩和海马萎缩的情况下,评估了各组中区域WMH体积和认知能力之间的横断面关系。
他们发现:与Aβneg-对照组相比,Aβpos-AD患者所有区域的WMH体积都较大,其中胼胝体压部(S-CC)的变化最大。
在Aβpos-AD患者中,总的和区域性的WMH体积较大,特别是在S-CC,与认知能力下降密切相关。
这个研究的重要意义在于发现了 :WMH是导致AD患者认知能力下降的主要原因,与淀粉样蛋白沉积和萎缩无关。这项研究强调了WMH在AD中的临床意义,尤其是后部WMH,最明显的是S-CC的WMH。
原文出处:
Garnier‐Crussard A, Bougacha S, Wirth M, et al. White matter hyperintensity topography in Alzheimer’s disease and links to cognition. Alzheimer’s & Dementia. Published online July 28, 2021:alz.12410. doi:10.1002/alz.12410
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#白质#
44
#ERS#
52
#alzheimers#
55
#dementia#
56
#高信号#
43
#MERS#
40
#白质高信号#
43
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
65