JVS:小儿急性髂股动脉血栓形成抗栓治疗的自然病程
2020-10-29 《门诊》杂志 门诊新视野
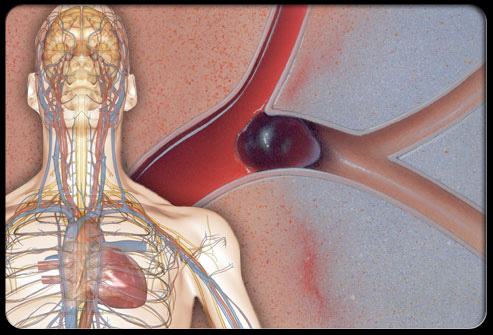
急性髂股动脉血栓形成(IFAT)可发生在危重新生儿和婴儿中,这些患儿需要动脉留置针进行监护或因心导管术造成的结果。指南建议使用抗凝治疗,但支持最佳治疗时间和超声(US)监测作用的证据有限。本研究[1]
急性髂股动脉血栓形成(IFAT)可发生在危重新生儿和婴儿中,这些患儿需要动脉留置针进行监护或因心导管术造成的结果。指南建议使用抗凝治疗,但支持最佳治疗时间和超声(US)监测作用的证据有限。本研究[1]的目的在于描述血栓溶解动力学,并确定合适的抗凝时间和监测间隔。
研究方法
这是一项单中心回顾性队列研究,研究对象为2011年至2019年期间患有急性IFAT的儿童。回顾了医疗记录和血管实验室的研究。纳入US监测≥1次的患者。研究者将血栓的溶解定义为经超声检查证实腔内无物质回声。采用Kaplan~Meier(KM)分析评估血栓的溶解时间。
研究结果
50例患者的54条肢体被确诊为急性IFAT。中位年龄9.9周(IQR:3.1~21.7),中位体重4.2 kg(IQR:3.3~5.5)。急性IFAT患者的肢体(65%)大部分表现为足部多普勒超声减弱,多见于心导管术后(55%)。48条(89%)肢体动脉完全闭塞,其中48%在踝关节以下未见血流。每条肢体接受US的中位次数为3(范围:2~7),61%的肢体在诊断后7天内进行了US监测。抗凝治疗后,有33%和64%疗的患者,预计分别在14天和30天内血栓完全溶解。9例(17%)患者未接受抗凝治疗,其中仅2例患者IFAT溶解。诊断时,一名患者因抗凝禁忌症接受了开放性血栓切除术,另一名患者接受了溶栓治疗。没有组织丢失或截肢的病例。
总 结
对IFAT进行抗凝治疗获得了成功的短期疗效。根据观察到的溶解率,应在开始抗凝治疗后每隔两周监测一次。当使用抗凝治疗时,每两周就有1/3的患者有望溶解血栓。
原始出处:
Joel L. Ramirez, Christina Kuhrau, Bian Wu, et al. Natural History of Acute Pediatric Iliofemoral Artery Thrombosis Treated with Antithrombotic Therapy. Journal of Vascular Surgery. 2020. DOI: https://doi.org/10.1016/j.jvs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了
34
#股动脉#
31
#自然病程#
37
#动脉血#
29
#动脉血栓#
48
#动脉血栓形成#
29
#动脉血栓形成#
35