The Lancet Rheumatology:与急性膝关节损伤2年后结局相关的临床和分子特征:来自肯尼迪膝关节损伤队列的纵向研究(KICK)结果
2021-09-10 MedSci原创 MedSci原创
关节损伤是骨关节炎的主要危险因素,这为前瞻性探究骨关节炎相关的早期过程提供了机会。这篇文章调查了基线人口特征和临床因素,以及膝关节滑液和血浆或血清中的蛋白质是否与膝关节损伤后2年后的临床结局相关。
关节损伤是骨关节炎的主要危险因素,这为前瞻性探究骨关节炎相关的早期过程提供了机会。这篇文章调查了预定义的基线人口和临床因素,以及膝关节滑液和血浆或血清中的蛋白质是否与膝关节损伤后2年后的临床结局相关。
这项纵向队列研究在2010年11月1日至2014年11月28日期间招募了英国伦敦六家医院和诊所的16-50岁的患者。受试者在8周内曾有严重的急性膝关节损伤(MRI上显示积液和结构损伤),通过手术治疗。对受试者测量的预定义基线临床变量包括从受伤到采样的时间、受伤的程度和类型、滑液血染色、有无积液、自我报告的性别、年龄和 BMI,此外还在基线和3个月时通过免疫测试检测12种滑膜液标志物和四种血浆或血清生物标志物。主要结局是所有患者校正基线评分后的2年时膝关节损伤和骨关节炎结果评分 (KOOS4)。使用针对预定义协变量进行调整的线性和逻辑回归模型来评估基线变量和2年后 KOOS4的关联性。该研究在 ClinicalTrials.gov注册,编号为 NCT02667756。
该研究纳入150 名患者,膝关节损伤后中位时间为17天(范围1-59天,四分位间距9-26天)。123名(82%)为男性,中位年龄为25岁(范围16-50岁,四分位间距21-30岁)。150名参与者中有98人(65%)完成了入组2或3年后 KOOS4评估(50名参与者失访,2人因与研究无关的不良事件退出);77名(51%)参与者拥有所有必要变量,被纳入到核心变量调整分析中。在2年的数据集中,平均KOOS4从基线时的38(SD 18)提高到两年后的79(18)。基线KOOS4、中到大量膝关节积液、中重度滑膜血染色及其相互作用显著预测2年KOOS4(n=77;系数-20.5,95%CI -34.8至-6.18;p=0.0060)。与2年KOOS4 独立相关的预定义生物标志物是滑液 MCP-1(n=77;-0.015, 0.027到-0.004每变化1 pg/mL单位;p=0.011)和IL-6 (n=77;-0.0005,-0.0009到-0.0001每变化1 pg/mL 单位;p=0.017)。这些生物标志物,结合关节积液和血液染色的相互作用能解释39%的结果变异性。试验中发生了两个与研究相关的不良事件,都发生在采血时(一个是晕厥前发作,另一个是静脉穿刺部位的压痛和疼痛)。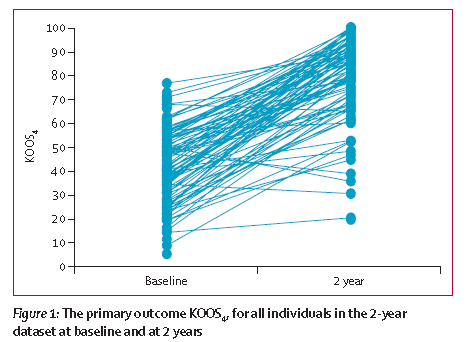
结论:关节积液和积血与急性膝关节损伤后的症状性结局显著相关。急性膝关节损伤后的滑液分子蛋白变化(最佳代表为MCP-1和IL-6)与症状性结局独立相关,但与结构性结局无关。与临床预测因子相比较,生物标志物总体上起次要作用。需要更好地了解急性膝盖损伤后的结构及其症状之间的关系,以及此过程早期的明显分离从而取得临床进展。
出处:
Garriga C, Goff M, Paterson E, Hrusecka R, Hamid B, Alderson J, Leyland K, Honeyfield L, Greenshields L, Satchithananda K, Lim A, Arden NK, Judge A, Williams A, Vincent TL, Watt FE. Clinical and molecular associations with outcomes at 2 years after acute knee injury: a longitudinal study in the Knee Injury Cohort at the Kennedy (KICK). Lancet Rheumatol. 2021 Jun 24;3(9):e648-e658. doi: 10.1016/S2665-9913(21)00116-8. PMID: 34476411; PMCID: PMC8390381.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#纵向研究#
26
#分子特征#
30
#Lancet#
30
#Rheumatology#
24
#损伤#
32
顶刊就是不一样,质量很高,内容精彩!学到很多
45